I had the fortune of attending ISPAD 2024 in Lisbon, Portugal. The pace of the research into the screening and prevention of type 1 diabetes is mind-boggling! The spotlight was well and truly shone on type 2 diabetes in children. Finally, research into GLP-1’s for both type 1 and type 2 diabetes shows promise. Here are my seven take aways.
1. Delaying progression to T1D Stage 3
The ADA consensus guidelines recommend early identification of T1D stages 1 and 2, as it opens an important opportunity for education and preparation for reducing DKA and subsequent morbidities, developing glycemic management skills, and avoiding hospitalisation. Also, the guidelines highlight for those identified: 1. monitoring measures of glucose regulation every three months; 2. measuring random venous or capillary blood glucose simultaneously with A1c levels; 3. using OGTT as the method of choice to assess T1D stage; and 4. referring to specialists in T1D progression for discussion of risk and options for monitoring wherever feasible.
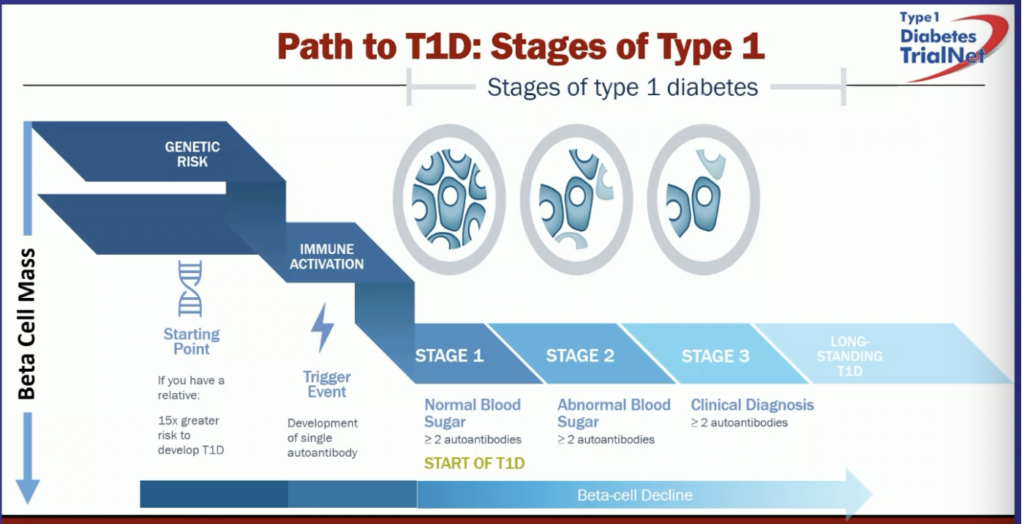
The Fr1da study shows that 90% of the people identified with stage 2 T1D did not have a first-degree relative with T1D. Therefore, this highlights the need for a nationwide screening programme. Tzield (teplizumab) is licensed for 8 years and above after showing a 2-3 year delay of progression to T1D stage 3. Tzield is undergoing a NICE appraisal. Further trials are being undertaken on children aged 2-8 years.
Colin Dyan from Cardiff discussed the multiple immune-modulating agents being tested for delaying T1D progression. He envisages a future where various agents may be used over a time-course of years to achieve much longer delays in preventing T1D progression. For this to happen C-Peptide preservation has to recognised as a regulatory accepted end-point. Dr Dayan discussed the new clinical trials format that will allow multiple agents to be tested with only one control group, thereby speeding up science and getting cost-effective answers – the format is called T1D Plus.
Dr. Tabitha Randell discussed preserving pancreatic function. Infusion therapies (e.g., teplizumab, ATG, rituximab, abatacept, alefacept, golimumab), subcutaneous injections (e.g., ustekinumab, imatinib), and oral medications (e.g., baracitinib, verapamil). Future trials will give greater insight including JAKPOT T1D, T1D RELAY, Protocol TN-25, and TOPPLE T1D.
Dr. Randell also identified key challenges in T1D prevention and intervention:
- Identifying whom to screen.
- Genetic risk assessment and autoantibody testing – which ones and when
- What are the most effective ages for screening, 2-4 and 6-8?
- Integrating screening into routine practice
- Identifying candidates for novel treatments and clinical trials.
- Preventing DKA by adequate follow-up
2. AID from Diagnosis or Within 3 Months
Simply, for the vast majority of children diagnosed with T1D, the sooner they start an AID system, the better their control will be at 1 year and further still at 2 years.
Study: The CLOUD trial evaluated the benefits of AID systems for newly diagnosed children with T1D. It compared AID systems to traditional multiple daily injections (MDI) regimens in a randomized controlled trial with over 100 children.
Outcome: AID users achieved 73% Time in Range (TIR) compared to 60% for those on standard therapy. The AID system significantly reduced glycemic variability and insulin dosing errors, showing reduced risk of hypoglycemia and improved long-term glycemic control, particularly in the crucial first months post-diagnosis.
This is of the utmost importance considering tight control early in the course of T1D helps reduce the long-term risk of microvascular and macrovascular complications, as shown in the DCCT and EDIC data.
3. Metformin and Lifestyle for T2D will not be enough
The TODAY (Treatment Options for Type 2 Diabetes in Adolescents and Youth) and TODAY2 studies collectively provide a longitudinal analysis of youth-onset type 2 diabetes, highlighting the progressive nature of complications and the challenges in managing this condition over time.
Timeline and Key Findings:
1. TODAY Study (2004–2012):
• Objective: Evaluate the efficacy of different treatment options for maintaining glycemic control in youth aged 10–17 with type 2 diabetes.
• Treatment Groups: The study randomized 699 participants to three treatment regimens: metformin alone, metformin with rosiglitazone, and metformin with intensive lifestyle changes.
• Results:
• The failure rate in maintaining glycemic control was alarmingly high: 51.7% with metformin alone, 46.6% with lifestyle addition, and 38.6% with metformin and rosiglitazone.
• Takeaway: All treatments showed high rates of failure, with youth experiencing a faster progression of type 2 diabetes than typically seen in adults. The study highlighted the challenges of managing the disease effectively in this age group.
2. TODAY2 Study (2012–2020):
• Objective: Follow-up on the participants from the original TODAY study to assess the long-term health outcomes and the development of diabetes-related complications.
• Findings:
• By the end of the TODAY2 study, participants (mean age 26 years) had high rates of complications. For example:
• Hypertension: 67.5% had developed high blood pressure.
• Kidney Disease: 54.8% showed signs of diabetic kidney disease.
• Neuropathy: 32.4% developed nerve disease.
• Retinopathy: 51% had eye complications, including some advanced cases.
• Multiple participants developed severe cardiovascular issues, such as heart failure, which is highly unusual for this young age.
• Key Insights:
• The majority of participants had at least one major complication, with 28.4% suffering from two or more.
• The clustering of complications in this population demonstrated the aggressive nature of youth-onset type 2 diabetes and the urgent need for more effective treatments and preventive care strategies
Overall Implications:
The combined findings from the TODAY and TODAY2 studies underscore that youth-onset type 2 diabetes progresses rapidly and is linked to severe, early-onset complications. These include kidney disease, nerve damage, and cardiovascular issues that typically appear much later in adults with type 2 diabetes. Both studies stress the need for early intervention, aggressive management, and the development of better treatment approaches to reduce the high rates of glycemic failure and long-term health complications. Furthermore, Dr Dezer presented complication rates of youth living with T2D from the German DPV registry. The DPV registry showed even higher incidence and progression of both micro and macro vascular complications than the TODAY study.
4. Adding SGLT-2 Inhibitors or GLP-1 Agonists in T2D
Study: The AWARD-PEDS trial (n=154) assessed the efficacy of dulaglutide (a GLP-1 receptor agonist) in children with T2D while the DINAMO trial (n=158) explored the effects of dapagliflozin (an SGLT-2 inhibitor).
Outcome: Dulaglutide reduced A1c by 1.1% over 26 weeks, while dapagliflozin decreased A1c by ~0.8% in adolescents with T2D. Both treatments were well-tolerated. The addition of these agents can provide better metabolic control and potentially reduce the risks of long-term complications associated with poorly controlled diabetes.
In obese youth (without T2D), a Semagluatide trial showed significant weight loss compared to placebo and may offer a route for T2D prevention and remission. We are awaiting further trials on T2D in youth due to be published next year.
Updated ISPAD guidelines for T2D are imminent and will recommend Metformin and lifestyle first and basal insulin if A1c is above 69 mmol/mol. However, it is imperative to try to wean off insulin ASAP and replace with a GLP-1 or SLGT2. If metformin and lifestyle cannot achieve A1c <48 mmol/mol, instigate GLP-1 or SLGT2 early.
5. Obesity Management Using Height-to-Waist Ratio
This study explored the relationship between waist-to-height ratio (WHtR) and insulin resistance in overweight/obese children. WHtR tertiles were divided by sex:
Males: T1 ≤ 0.55, T2 > 0.55–≤ 0.59, T3 > 0.59
Females: T1 ≤ 0.56, T2 > 0.56–≤ 0.6, T3 > 0.6
Children in the highest WHtR tertile (T3) had significantly higher risks of insulin resistance and elevated liver enzymes compared to those in lower tertiles. The study suggests that WHtR can serve as a practical screening tool for metabolic syndrome in children.
The role of early intervention is crucial, as pediatric obesity worsens insulin resistance, increasing the risk of rapid-onset type 2 diabetes complications such as hypertension, dyslipidemia, and cardiovascular events. It may also serve as a more sensitive marker of intervention success.
6. Time in Tight Range (TITR) for Well-Controlled Patients
Study: A real-world analysis of pediatric AID users in Italy (n=613) focused on TITR as a potential key metric for tighter glycemic control. The study tracked outcomes in children on the MiniMed 780G and Control-IQ systems.
Outcome: The cohort achieved an average TITR of 47%, with top quartile users reaching over 50%. The study showed that TITR, while more aggressive, could be safely achieved without increasing the risk of hypoglycemia (TBR remained under 4%). This shift toward tighter glucose control could help prevent long-term complications such as retinopathy or nephropathy.
The clinical suggestion is to aim for 50% TITR if the person is achieving 70% TIR. If not achieving 70% TIR, then an additional target may increase anxiety from unrealistic expectations. Furthermore, for the majority to achieve TITR, a second agent such an SLGT2, GLP-1, or Amylin may be needed to help control post-meal hyperglycaemia. BREAKTHROUGH T1D is currently funding several of these trials.
7. Exercise and T1DM and T2DM
Children with T2DM have much lower VO2 max and ability to burn fat due to insulin resistance, therefore, they often find moderate-intensity physical activity very hard. There is a need to start at a low intensity and increase gradually. Using a GLP-1 or SLGT2 as the second-line agent may allow for better adaptations to physical activity.
There is an upcoming EASD/ISPAD consensus statement on AID systems and exercise for T1D, with generic recommendations, AID device-specific recommendations, and suggestions for specialty circumstances with easy-to-follow infographics. Considering I am one of the authors, I will write a summary once published to get across the key messages.
I share this information with those who subscribe for informational purposes only.

