Adhering to the principle of skin in the game, I spent over seven years (2017 to 2025) acquiring personal and professional experience before putting pen to paper for this comprehensive guide.
Sound too intense?
If so, I have created a more entertaining guide, comparing the systems to superhero’s.
Choosing an AID System: Which Superhero Do You Want in Your Corner?
Want to listen to the podcast on this?
Episode 1: Choosing Your AID Superhero. We compare the top AID systems to superheroes, helping you find the one that best suits your diabetes management style—whether you need control like Spider-Man, power like Hulk, strategic adaptability like Batman, or sleek automation like Iron Man.
Still here?
Great, here’s the comprehensive guide.
I have tried and tested the Medtronic 670G and 780G, T-Slimx2 with Control IQ, Omnipod 5, DIY Looping, and Android APS.
At work, I have helped 300 children and young people start on all of commercially available AID systems.
Quite simply, they are all game-changers!
It’s like picking a supercar, there is no “best AID system” just the “right AID system for you.
Some prefer a Porche, others a Lamborghini, and others a Ferrari.

Are you are employed in the healthcare sector or a person who loves the detail?
If so, after completing this guide try the AID System Study Day which details all the systems, provides workbooks and clinical tools, and has management sessions by world leading experts on nutrition, exercise, alcohol, optimising time in range, reviewing downloads, under 5’s and much more.
However, for most, this guide has what’s needed to make an effective choice and get the most out of the system selected.
This guide helps:
- Understand what AID systems are and how they work at a basic level
- Have simple decision-making criteria when selecting an AID system
- Acquire tips and tricks to get the most out of each AID system.
What are AID systems and how do they work, at a basic level?
AID systems have three components:
- An insulin pump
- A CGM device
- An algorithm that drives automatic insulin adjustments to stop highs and lows that is in the pump, or a SMART phone APP
Here are the current commercially available systems available (March 2025):
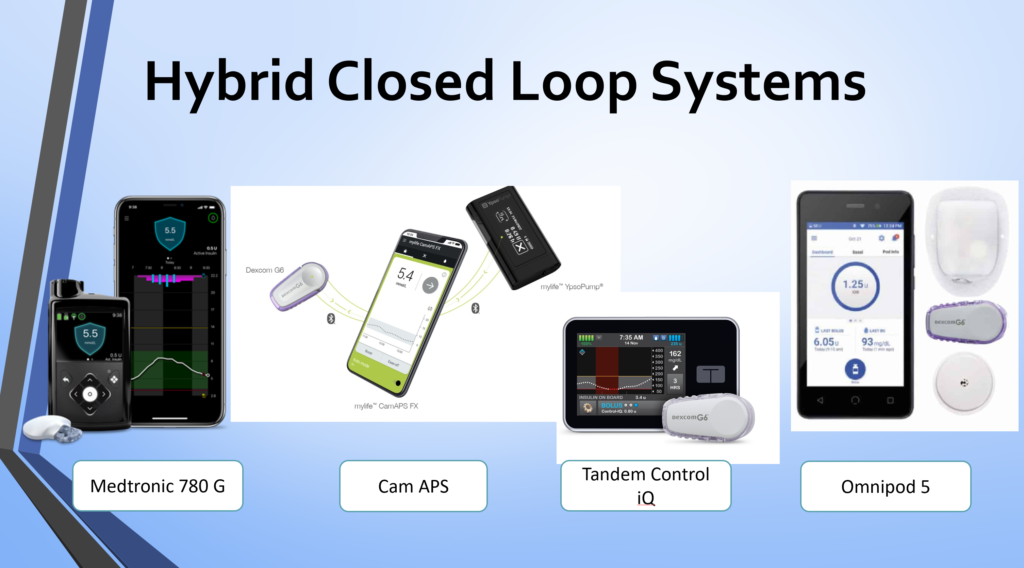
- Medtronic 780G
- T-Slimx2 with Control-IQ
- CamAPS FX
- Omnipod 5
- A range of unregulated Do It Yourself (DIY) options:
All AID systems have pros and cons, which we will get into shortly, however, they operate similarly.
- If the glucose level is predicted to rise above the target level, the algorithm calculates how much extra insulin is required to stop the glucose in its tracks. It gives extra insulin by increasing the pump basal rate or delivering an automatic correction bolus.
- If the glucose level is predicted to fall below the target level or into hypoglycaemia, the algorithm slows down the basal rate or stops insulin delivery.
- The user must enter all carbohydrates eaten and deliver a food bolus for the carbs. AID systems are not yet clever enough to allow eating without food bolus insulin. So the foundations of three balanced meals, accurate carbohydrate counting and delivering food insulin 10-20 minutes before eating still apply!
A picture paints a thousand words.
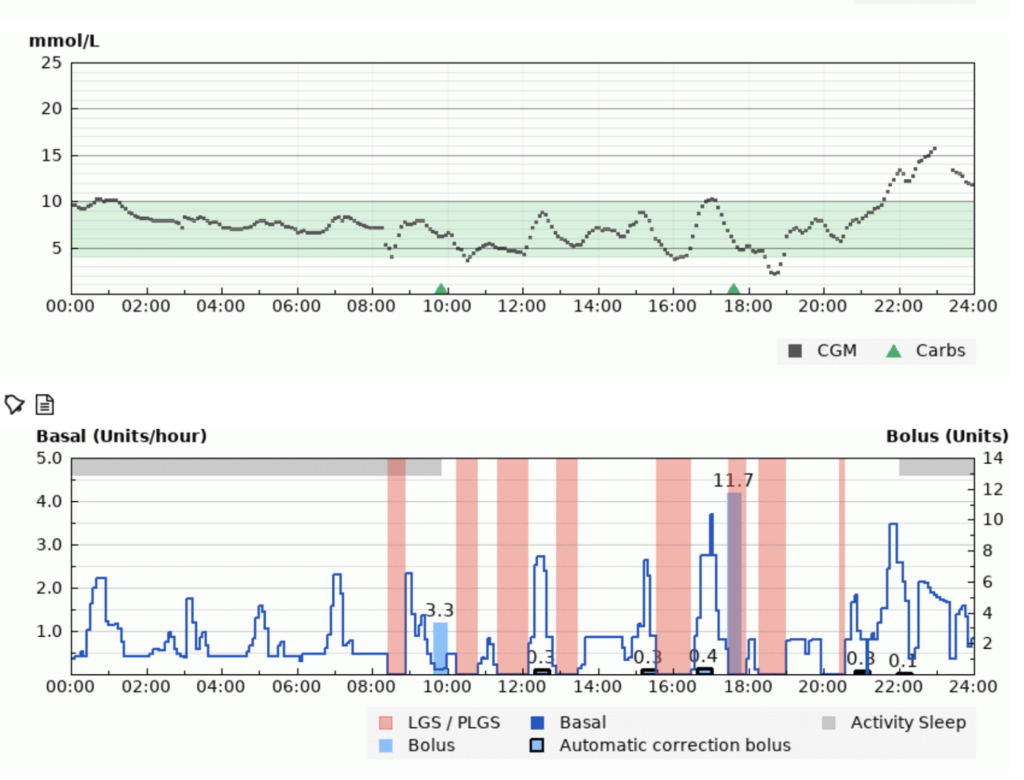
In the above example, you can see the CGM trace on the top and the insulin delivery on the bottom.
How does the algorithm increase insulin?
Overnight, when the glucose level is above the target level, the algorithm increases basal insulin to bring it back to target. Also, at 16:30 when the glucose is rising rapidly and predicted to go relatively high, the algorithm automatically corrects with 0.4 units of bolus insulin.
How does the algorithm decrease insulin?
During the day, you can see lots of pink bars representing where the basal insulin has been suspended to stop an episode of hypoglycaemia. Just before the pink blocks, the basal insulin has been slowed down.
The eagle-eyed of you will notice that this person had given a bolus for breakfast at 09:49 and the evening meal at 17:36. Those are the light blue bars of 3.3 and 11.7 units, respectively. Like is said, you still gotta bolus for those carbs!
What improvement in diabetes control can I expect using an AID system?
This graph summarises the expected benefit in terms of numbers.
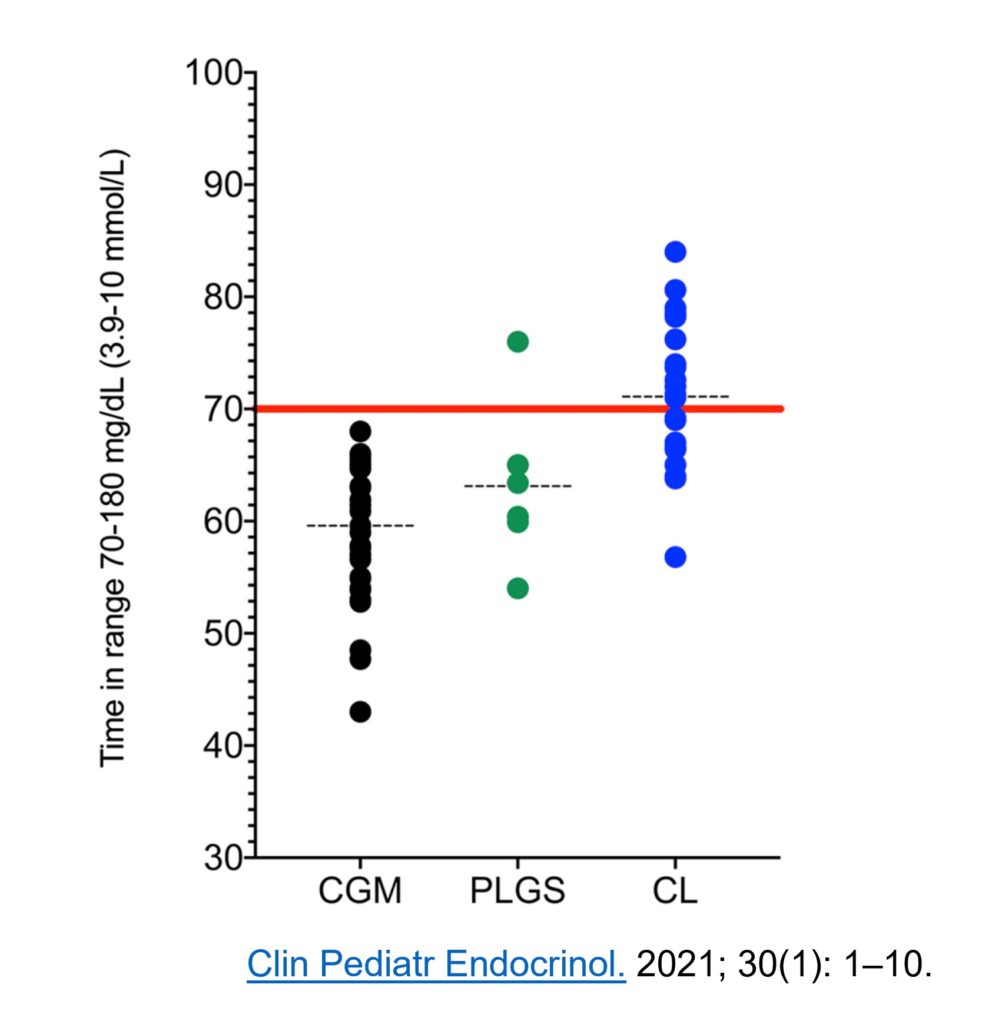
- All the studies using CGM represented by black dots show on average you can expect about 60% time in range (3.9-10.0 mmol/L or 70-180 mg/dL).
- Time in range does not improve much when pumps can suspend insulin to prevent lows, the green dots (PLGS).
- When the ability to increase insulin is added to become a closed-loop (CL), or as we are calling them AID systems, the time in range jumps to above 70% with the possibility of more than 90%.
- From my clinical experience, a user can expect to increase their time in range by 10-30% from their before AID system time in range. The lower your starting time in range, the bigger the increase, and vice versa.
What in life gives you more for doing less?
This 10-30% improvement is achieved with less daily diabetes management, not more!
Normally, to achieve more than 70% or higher time in range, a person with diabetes must:
- Check their CGM 20-50 times per day
- Give multiple correction bolus’s
- Swallow lots of glucose to prevent hypos
- Keep a detailed log of events and continually learn through trial and error
I must confess, I love this part of diabetes because I am a trial-and-error nerd!
However, this can quickly lead to diabetes burnout, frustration, and eventually giving up.
In life, there are seldom things that reach the promised land;
Getting more by more by doing less!
AID systems are one such example – A triumph for human ingenuity!
The main thing that makes AID the dog’s danglers is……
You get your 8 hours of sleep back!!!
No more hypos overnight.
No more waking with highs.
Flat CGM lines overnight and waking rested, both parents and people with type 1!
Now that you understand what AID systems are and the benefit you can expect, it’s time to think about how to choose the right system.
Before we do that please understand this.
All AID systems will improve your glucose control and quality of life.
Therefore, if you do not have access to certain AID system, do not stress.
They all do a great job and will get you that 10-30% improvement time in range with less diabetes hassle! Remember the supercar analogy?

So get your rose-tinted glasses on and work your way through the three questions that will help you decide what’s right for you.
Check out this section If you want a bit of fun comparing the systems to superhero’s.
Choosing an AID System: Which Superhero Do You Want in Your Corner?
For a deeper dive check this out.
