The amount of information on AID systems is overwhelming.
I know, it’s taken me six years to get my head around it. Trying to fathom which one to choose is a challenge.
Want to listen to the podcast on this?
Episode 1: Choosing Your AID Superhero. We compare the top AID systems to superheroes, helping you find the one that best suits your diabetes management style—whether you need control like Spider-Man, power like Hulk, strategic adaptability like Batman, or sleek automation like Iron Man.
I have condensed six years of learning to provide you with the most important questions to guide your decision:
- What AID systems are available to you?
- Which CGM device do you prefer?
- How much control do you want of the algorithm?
- How aggressive do you want the algorithm to be in preventing after-meal spikes?
There is no best system, only the best system for you. Don’t worry, you cannot make a bad choice, its just like choosing a super car!

So, work through these questions and see which one jumps out at you!
- What AID system are available to you?
The table below tells you what devices are needed for the different systems. Also, if they have European CE Marking. The table includes, as of March 2025, the license they have regarding age, weight, insulin brand, and total daily insulin dose (TDD).
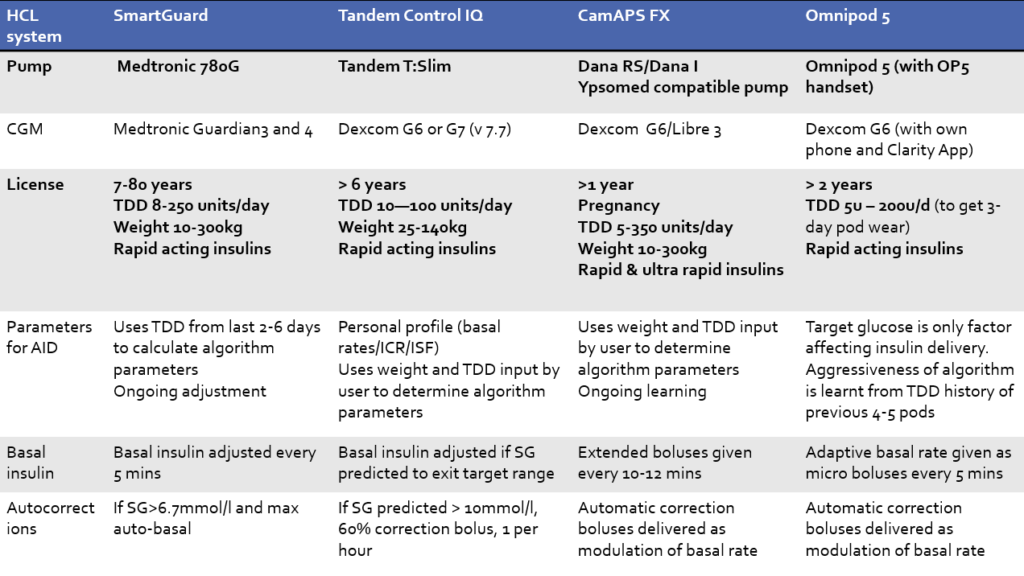
Just because they are commercially available in your part of the world and you fit the criteria, it does not mean they will be available in your country and diabetes centre.
You will need to ask your diabetes team.
The DIY options are not on the table here as they are not approved or regulated.
My current opinion is:
The commercially available AID systems are good enough for 99% of people with type 1 diabetes.
However, if you are in the 1%, a nerdy-obsessed person (like me) who wants 100% control and is happy to do the work required, go and check out what devices are compatible.
· Looping
· Open APS
Let us dig a bit deeper.
2. Which CGM device do you prefer?
If you are already using CGM you will have a bias to what you like. Use your own experience and go with what you like.
Pivotal question.
“Are you going to let a CGM device determine your insulin doses before you have tested it, and you are confident it’s accurate enough?”
It’s essential to understand how CGM accuracy is calculated if you want to make the best choice for YOU. To help, I have complied a CGM guide.
Also, also wrote a scientific paper assessing the accuracies of all sensors in 2023. After more research and sitting on the IFCC working Group for CGM, there are four clear winners for integration with AID Systems. The Dexcom G6 and G7 and the Freestyle Libre 2 Plus and 3 Plus.
The Dexcom G6 & G7 and the Freestyle Libre 2 & 3 Plus’s are the only sensors with FDA iCGM approval (March 2025). To attain iCGM status, the accuracy of the sensor must reach a very high bar, tested on a wide age range of people with type 1 diabetes!
The Medtronic Enlite 4 and Simplera, used with 780G, do not meet the iCGM standards. However, the MiniMed 780G has excellent clinical trial data and is therefore an excellent and safe choice.
Remember, no CGM device is risk-free. They all have inaccuracies, especially during exercise and when the glucose is moving fast. Therefore, you will still need to occasionally do a finger prick. If in doubt, get the finger pricker out! You can then calibrate if required, if the CGM system allows.
Personally, I believe having the ability to calibrate is very helpful for those few times a month the CGM is off track.
But, use an ISO standard blood glucose meter that’s aligned with the CGM. Also, following perfect calibration technique is essential. Reading the first two points of the CGM bells and whistles tells all.
Optional calibration is why I use Dexcom CGM’s products over Abbott’s Libre CGM’s. Jude and Grace would use Dexcom too. Not because they are more accurate, they are not. It’s just the ability to get back on track when the sensor accuracy is way off. This happens a couple of times a month and calibrating at these times retains my confidence and stops annoying false alarms, especially overnight.
But, I am a freak when it comes to following the calibration essentials! I use a ROCHE Accu-Chek Guide meter (the most accurate and reliable) that’s closely aligned with capillary glucose. For calibration samples;
“I wash my hands, dry them very well, milk (not squeeze) the finger, wipe away the first drop, take two tests, a third if they are not within 0.5 mmol/L (10 mg/dL) of each other, then average the results to for my final blood glucose value to calibrate my sensor with!”
Don’t calibrate unless you are prepared to be as militant as this! Otherwise you are likely to make the sensor less accurate.
3. How much control do you want over the algorithm?
This is a fundamental question, so take some time to think.
Do you want the system to do 90% of the heavy lifting by constantly updating the settings?
If yes, the best choices are the Medtronic 780G, CamAPS FX, or Omnipod 5.
All you must do is enter minimal settings and the target glucose level you want the algorithm to aim for!
You only need to keep your carb ratios up to date, and the algorithm takes care of the rest. This means you are not reliant on yourself or your diabetes team to update settings such as basal rates and correction factors correctly.
These systems reduce user error and minimise diabetes hassle.
However, if you are a person who has different sensitivities to insulin on different days, this can cause some problems.
For example, if you are not very active during the week but extremely active on the weekend, it’s likely the algorithm will be too strong on the weekend. Do you suffer from a wicked dawn or dusk phenomenon, if so, these systems may not not be able to meet your varying insulin needs.
Another example is if you are on medications that spike the glucose levels that you take sporadically, such as steroids, the algorithm will struggle to be able to keep up. There are some limited settings to help with this on these systems.
Finally, if you are a person who likes to tinker, you will not be able to do this.
Alternatively, do you want control of how the algorithm works and the flexibility to adapt as necessary?
If yes, the best choices are T-Slimx2 with Control IQ
Control IQ requires the user to set and regularly update the basal rates, correction factors, and carb ratios.
For adults, this usually means working hard for the first two weeks but only infrequent adjustments to fine-tune after that.
For children, this means getting the initial settings on point and regular updates every three months or so.
The long-term success of these systems is reliant on the user and the diabetes team who support them. However, Control-IQ offers ultimate flexibility.
As Uncle Ben says to Peter Parker (Spiderman) “With Great Power Comes Great Responsibility”.
For example, you can have a different profile of settings for weekdays and weekends, holidays, and importantly, a night out drinking alcohol.
Also, you can make settings much more aggressive for times of illness or medications.
Reading this I am sure you will know which camp you’re in.
Final question.
4. How aggressive do you want the algorithm to be in preventing after-meal spikes?
The major limitation of all AID systems is that they use “Fast Acting” insulin.
This is misleading because the “Fast-Acting” insulins are not as fast as the carbohydrate absorption from meals.
This means glucose spikes after eating high carbohydrate meals still happen when using AID.
Of course, you want to do the basics of eating balanced meals, carb counting accurately, and giving insulin 10-20 minutes before eating.
However, we all know this is not possible 100% of the time.
How effective AID systems are at tackling after-meal glucose spikes depends on two things:
- Target level
- The aggressiveness of the algorithm
This table shows the different target levels and adjustable settings that impact the AID algorithms. Very simply, the lower the target can be set, the quicker the algorithm will start increasing the insulin.
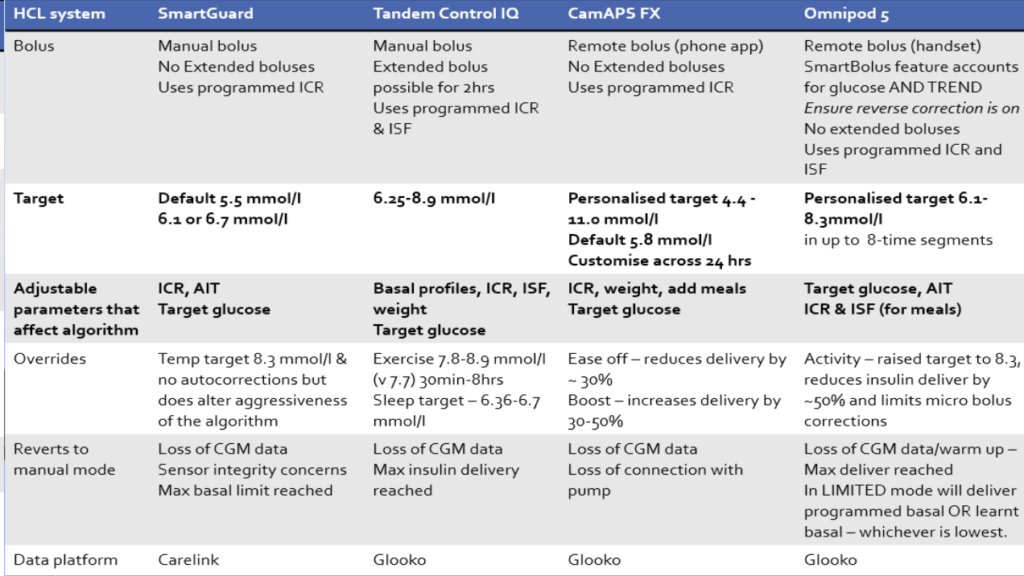
From the lowest to highest tar:
- CamsAPS FX – 4.4mmol/L is the lowest and multiple time blocks (up to 48) can be set.
- 780G – 5.5 mmol/L is the lowest but must have that setting for the whole day, with no flexibility.
- Omnipod 5 – 6.1 mmol/L is the lowest with up to 8 time blocks
- T-Slimx2 with Control-IQ – Does not increase insulin if predicted to be within 6.25-8.9 mmol/L in the next 30 mins
The second consideration is if you can adjust the algorithm settings to make it more aggressive.
It comes down to active insulin time and correction factor.
Active insulin time is the duration the algorithm thinks the insulin lasts. When insulin is given for food or corrections, the algorithm uses active insulin time to calculate how much insulin on board there is that might drop the glucose level. This is then used in the calculations of how much extra insulin to give to tackle highs. The shorter you set it, the more aggressive the algorithm will be.
From most to least aggressive:
- 780G (if active insulin set 2 or 2 ½ hrs)
- Omnipod (2hrs aggressive, 2.5 hrs normal, 3 hrs safe)
- CamsAPS FX (calculated by artificial intelligence)
- T-Slimx2 with Control-IQ (fixed at 5 hrs)
The Correction Factor (CF) or Insulin Sensitivity Factor (ISF) is the setting that tells the algorithm how sensitive the user is to insulin. If set aggressively, the alorithm will correct with lots of insulin. If set conservatively, the algorithm will be mild in correcting with extra insulin.
In order of ability to alter correction factors to alter the aggressivness.
- T-Slimx2 with Control-IQ – set by the user and can have multiple time blocks
- Omnipod – the Correction Factors in the algorithm are automatically calculated. However, the user sets Correction Factors in the bolus calculator that are employed when the user gives a correction via the Bolus calculator, even when Smart Adjust is running.
- CamsAPS FX and 780G (calculated by artificial intelligence)
There is a trade-off to consider.
The more aggressive the algorithm is the fewer highs but the potential increased risk of lows.
There we have it.
First, find out what’s available.
Second, think about what CGM sensor you want to use.
Third, consider how much hassle or flexibility you want from the algorithm.
Finally, ponder how you can alter the settings to adjust the aggressiveness of the system.
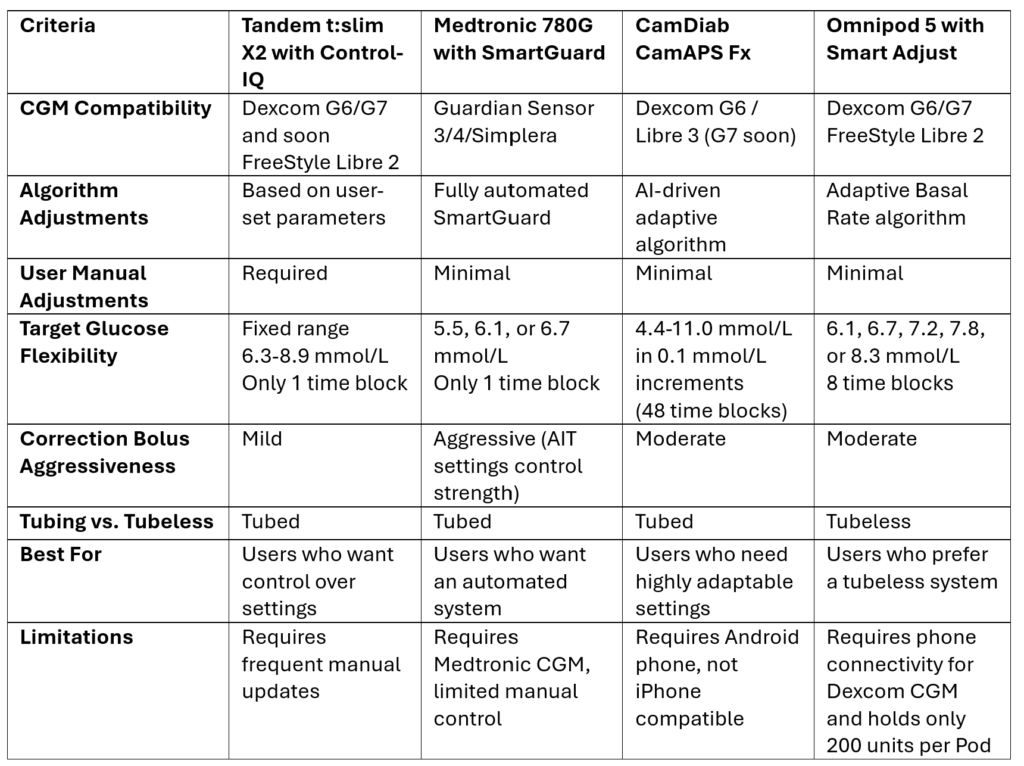
Here is a comparison table based on the criteria
Great, you have made your choice.
It’s time to access the tips and tricks for your system
