If you live with T1D and are choosing to drink alcohol, please check in with your diabetes care team and have support in place. This is not medical advice.
Alcohol carries real risks, physical, emotional, and social, and should always be treated with respect. But because it’s so common, and because it can significantly affect blood glucose levels, it deserves careful attention in this guide.
Alcohol is the most commonly used recreational drug, woven into many social and cultural traditions long before legal systems attempted to regulate its use. Whether it’s drinks at a wedding, beers at the pub, or cocktails on a night out, alcohol is present in a lot of people’s lives, including those of us living with T1D.
I’ve had some of the best nights of my life while drinking alcohol. But I’ve also woken up in very severe hypoglycaemic states. I’m not proud of this! I didn’t plan properly or think things through. But it’s the reality. If I’d known what is written below at the time, I genuinely believe I could have avoided this very risky situation. Luckily, I was wearing T1D identification, which meant I got the right help quickly enough.
What Alcohol Does to the Body and Brain
Alcohol is classified as a depressant, meaning it slows down the central nervous system. But it doesn’t always feel that way at first. That’s because alcohol:
- Increases dopamine, a chemical that fuels motivation and pleasure-seeking — often leading to more dancing, socialising, and (for some) over-drinking.
- Increases GABA, an inhibitory neurotransmitter that slows brain activity. This is what causes the slurred speech, clumsy movement, and sedation when alcohol builds up in your system.
People react to alcohol in different ways. Some feel energised and sociable, while others become emotional, tired, or irritable. This isn’t just down to personality, it’s influenced by brain chemistry, life circumstances, and your personal relationship with alcohol. I’m usually a happy drunk who loves to dance, but if I drink when I’m not in a good mood, it can easily turn into an anxious and unpleasant night.
Why Alcohol Increases Hypo Risk
From a diabetes perspective, the key issue with alcohol is its impact on the liver. Alcohol is a toxin, and the liver treats it like a top priority. When alcohol is present, the liver stops doing one of its usual jobs: putting glucose into the bloodstream (a process called gluconeogenesis).
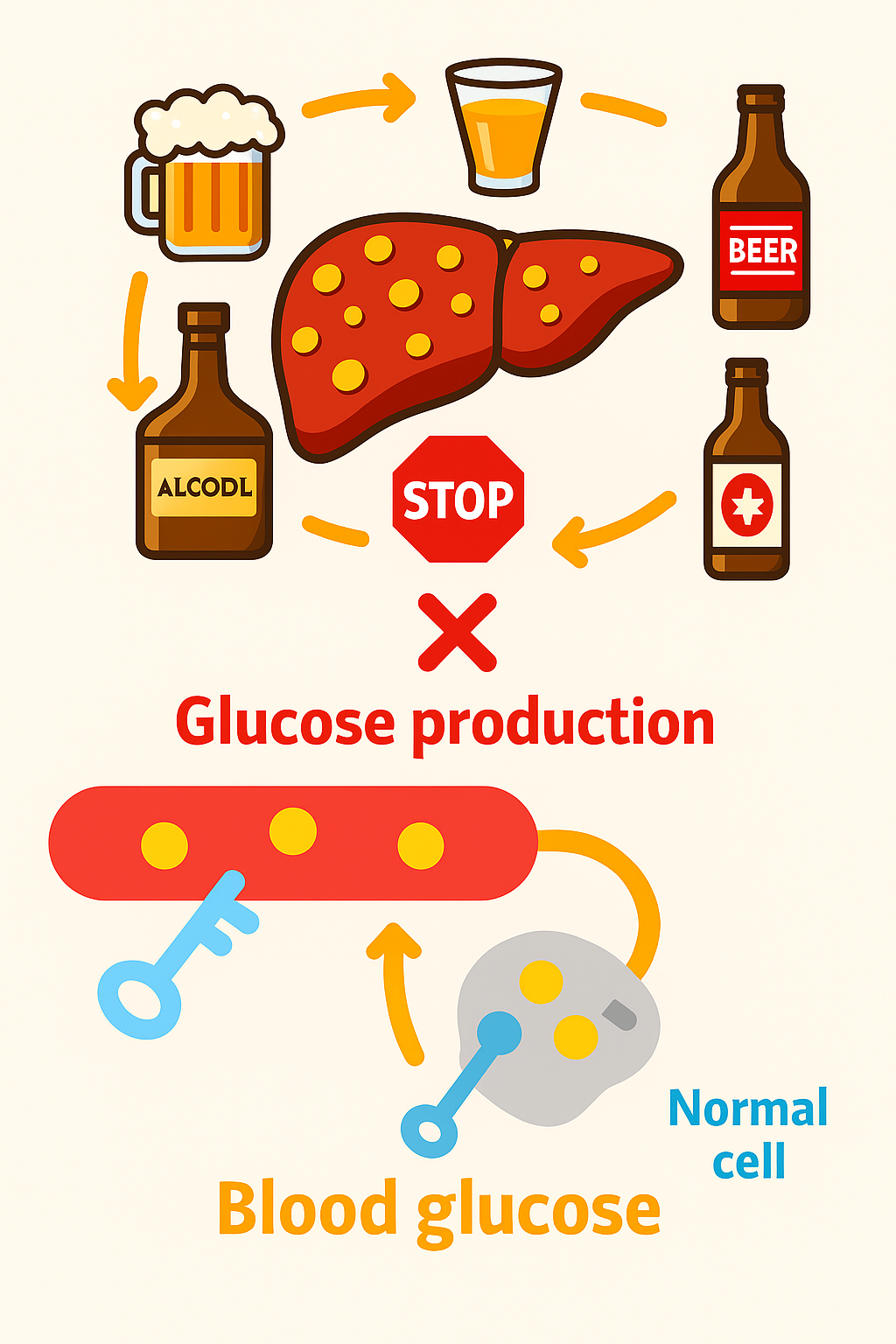
The liver reducing its usual glucose output is a major issue for people with T1D. Basal (background) insulin is designed to match the liver’s steady release of glucose, so when the liver slows or stops this output due to alcohol, but insulin remains active, blood glucose levels can fall. Making matters worse, glucagon is unlikely to be effective in this situation, because it works by triggering the liver to release stored glucose. Those stores can become depleted overnight, and the liver’s ability to produce new glucose (via gluconeogenesis) is impaired while it prioritises breaking down alcohol.
How do you know how long the liver stays impaired in making new glucose?
- 1 unit of alcohol = 1 hour of reduced liver glucose output and increased hypos risk
- 2 units (1 beer) = 2 hours
- 4 units (1 large glass of wine) = 4 hours
- 8 units (2 strong pints of beer) = 8 hours
- 12 units (bottle of wine) = 12 hours
- 20+ units (big night out with shots) = 20+ hours
The risk of hypos can extend well into the following day, depending on how many units of alcohol you consume. That’s why it’s important to have a rough idea of how much you’ve had, or plan to have, so you can take steps to reduce the risk. This is especially critical because when intoxicated, you may not wake up to the usual symptoms of low blood sugar or respond to CGM alarms. With larger amounts of alcohol, this risk can last even longer.
Key Questions to Ask Yourself
- How many units of alcohol will I consume?
- Will my drinks contain carbs?
- What insulin therapy am I using (MDI, pump, AID)?
- What’s my glucose level now and how am I trending?
- Do I have a plan for overnight and next-morning safety?
Drink Categories: Carb vs. No-Carb
Low/No-Carb Alcoholic Drinks (Minimal effect on glucose rise, higher hypo risk later).
I choose drinks that make it easier to manage my glucose levels, usually white wine with soda or spirits with diet mixers. If I’m being honest, in my late 20s to 40s, a typical night out could involve anywhere from 6 to 30 units of alcohol. That kind of intake significantly increases my risk of hypoglycaemia and often requires significant insulin reductions.
| Drink | Units per drink | Carbs (g) |
|---|---|---|
| Vodka + Diet Mixer | 1–2 | 0 |
| Gin + Slimline Tonic | 1–2 | 0 |
| White Wine (dry) | ~2 | ~1–2 |
| Red Wine | ~2 | ~1–2 |
| Tequila, Neat Spirits | ~1 | 0 |
| White Wine Spritzer | ~1.5–2 | ~2 |
Alcoholic Drinks with Significant Carbs (Pushes glucose up initially, then falls later).
I personally struggle with this because I don’t like letting my glucose run high, and I often end up over-correcting. But for others, allowing glucose to rise a bit and gradually drift down overnight can work well. Just be cautious if you’re using an AID system, automatic corrections and carb miscalculations can cause problems.
| Drink | Units per drink | Carbs (g) |
| Pint of Beer | 2–3 | 10–15 |
| Cider (dry) | 2–3 | 15–20 |
| Cider (fruity/sweet) | 2–3 | 30–40 |
| Alcopops / Ready-Mix | ~1.5–2 | 25–40 |
| Sugary cocktails | 1.5–2.5 | 20–40+ |
| Mixed shots + energy drink | 1–2 | 15–30 |
Insulin Strategies by Therapy
On MDI (Multiple Daily Injections):
- Pre-drinking: Reduce long-acting insulin by 25-75% if drinking 4-20+ units of alcohol
- During: Small snacks if glucose <7 mmol/L (126 mg/dL)
- If alcoholic drinks contain carbs consider a reduced bolus strategy (e.g., 0-50%), be very careful, and start low.
On Pump Therapy:
- Set temporary basal reduction (25–75%) before first drink until late morning, if drinking 4-20+ units of alcohol
- During: Small snacks if glucose <7 mmol/L (126 mg/dL)
- If alcoholic drinks contain carbs consider a reduced bolus strategy (e.g., 0-50%), be very careful, and start low.
On AID/Hybrid Closed Loop Systems:
- Activate Activity Mode before drinking and keep it on overnight, if drinking 4-20+ units of alcohol
- During: Small snacks if glucose <7 mmol/L (126 mg/dL)
- Be careful of auto-corrections after carb-heavy drinks — consider small insulin doses (0–50%) for the carbohydrate in drinks
Post-Drinking Hunger: What to Do
Late-night hunger is common. Your liver is craving fuel, and your brain is too. But be careful, this is where many people misjudge insulin.
Guidelines for Late-Night Eating
Golden Rule: If in doubt, don’t give insulin, but monitor and stay in Activity Mode on an AID system
| Glucose Level | Carbs Needed | Insulin Consideration |
| <7 mmol/L (<126 mg/dL) | 30g+ carbs | No insulin |
| 7–10 mmol/L (126–180) | 10–20g carbs | No insulin |
| >10 mmol/L (>180 mg/dL) | 0-10g | No insulin |
| If you’re eating more carbs, on top of the amounts suggested above, you may need a small amount of insulin but be cautious. | 0–50% insulin, be very careful, and start low. |
Glucagon, Medical ID, and Emergency Planning
Glucagon may not work after heavy drinking (8+ units), as alcohol stops the liver producing glucose (gluconeogenisis)
- Have medical ID on you at all times
- Let friends know you have T1D
- Consider CGM sharing and location sharing on your phone
Festival & Big Night Out Kit List
| Festival & Big Night Out Kit List |
|---|
| Glucose tablets |
| Fingerprick meter (CGM isn’t enough) |
| Backup CGM sensor (or two pre-inserted) |
| Medical ID bracelet/card |
| Fast-acting carbs (juice, sweets) |
| Water bottle |
| Insulin pens/syringes (even if on a pump) |
| Portable battery pack |
| Phone with CGM + location sharing on |
| Anti-nausea tablets |
| Spare cannulas |

Hope this was helpful
John
