If you live with T1D and are choosing to drink alcohol, please check in with your diabetes care team and have support in place. This is not medical advice.
This is Part 2 of the Partying with T1D guide. Part 1 explains the mental model to ensure safety when partying with T1D. This guide explains why alcohol is uniquely risky with T1D, how the risk shows up in real life, and what practical harm-reduction patterns people use.
Alcohol may not be your thing, and you may want to jump straight to Part 3: Stimulants or Part 4: Cannabis, Ketamine, and Hallucinogens.
System framing: alcohol is common, socially normalised, and often underestimated. But with T1D it can create a specific failure mode: delayed hypoglycaemia + reduced self-rescue. The risk is usually not “one drink”. It’s a bigger pattern: insulin on board, disrupted sleep, dehydration, late-night eating, and your liver being busy metabolising alcohol instead of supporting glucose stability. [1] [2]
Check out:
- Episode 25 — Alcohol with T1D with Dr Dessi Zaharieva
- FAQ — Alcohol and T1D
- Download the Alcohol & Type 1 Diabetes FAQ (PDF)
Overview
Alcohol is the most widely used recreational drug. It’s woven into weddings, pubs, festivals, dates, celebrations, and grief. People with T1D are part of that world, not outside it.
John has had some of the best nights of his life while drinking alcohol. He’s also had nights that ended in severe hypoglycaemia the following morning because I didn’t plan properly and didn’t understand the delayed risk. He’s not proud of that — but it’s real. This page exists so you can borrow lessons without paying the same price.
The detail
What alcohol does to the brain and body
Alcohol is classified as a depressant (central nervous system slowing), but the early effects can feel stimulating. Mechanistically, two common drivers are:
- Dopamine effects that can amplify motivation, reward-seeking, and “keep going” behaviour.
- GABA effects that increase inhibition in the brain, driving slurred speech, clumsiness, sedation, and reduced judgment as alcohol accumulates.
People react differently. Some become social and energised. Others become emotional, tired, or irritable. That variation isn’t just “personality” — it’s biology, context, and relationship-with-alcohol history. This matters in T1D because mood, appetite, and attention directly change glucose decisions.
Why alcohol increases the risk of hypos: the liver problem
From a T1D perspective, alcohol’s central issue is the liver. The liver prioritises breaking down alcohol, which can reduce its ability to release glucose and defend against falling glucose levels. This is why alcohol is strongly associated with delayed hypoglycaemia — often later in the night and the next morning. [1] [2] [3]
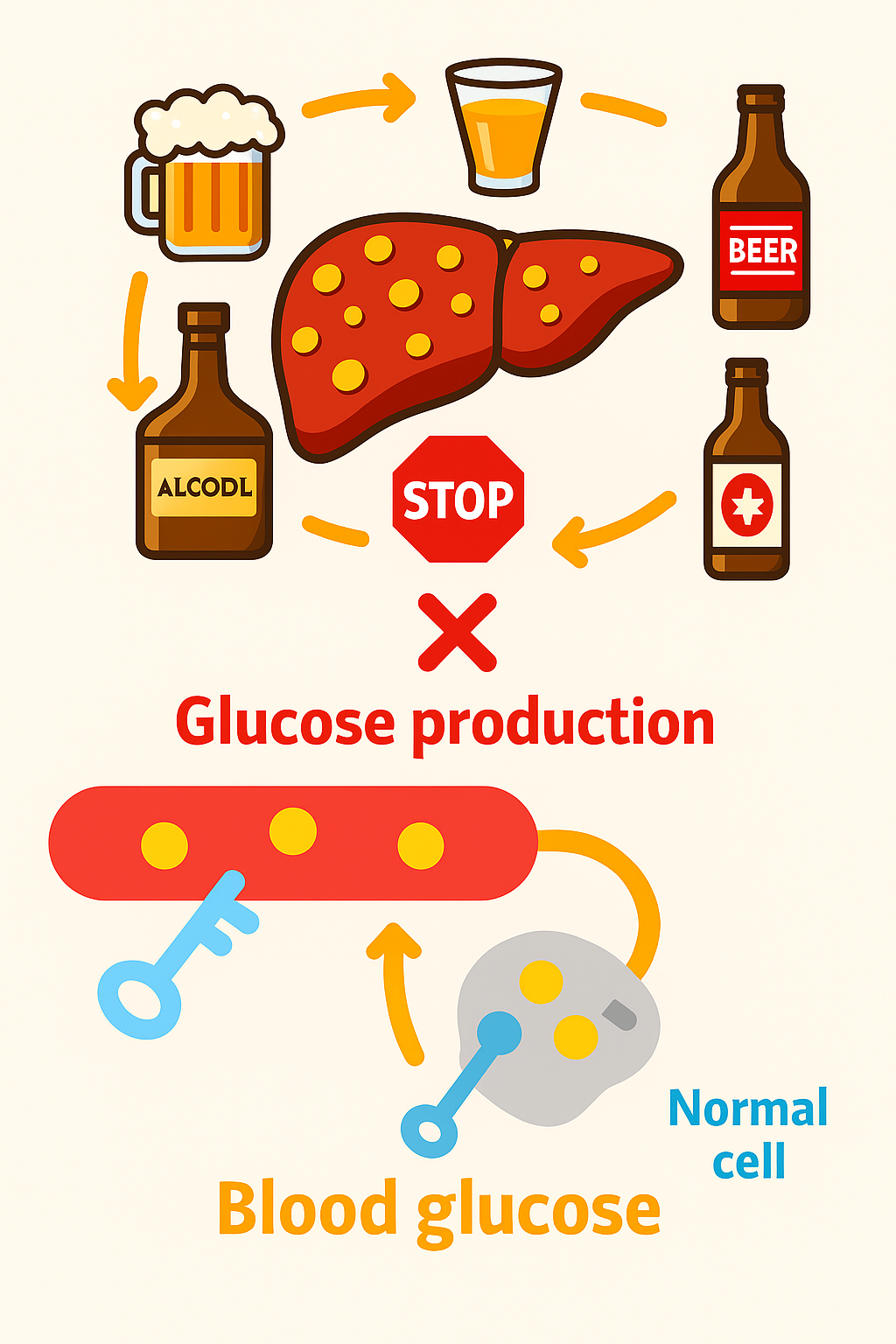
This is a mismatch problem: basal/background insulin keeps working, but the liver’s glucose support may be reduced. That mismatch can drive glucose down when you’re least able to notice it or treat it.
Important nuance: rescue tools can behave differently. Glucagon works largely through the liver. If the liver is busy and glucose stores are limited, glucagon may be less reliable than you expect after heavier drinking. This is one reason alcohol nights need an overnight plan, not just a “during the night” plan. [2]
How long does the risk last?
You will see rules online like “one unit = one hour”. Treat these as rough heuristics, not physiology. The real answer depends on body size, sex, liver function, food intake, sleep, hydration, activity, and how much insulin is active.
What we can say with higher confidence: delayed hypoglycaemia can occur many hours later, including the next morning, and sometimes well into the next day — especially after heavier drinking. [1] [2] [3]
The core questions to ask before and during
- Roughly how much alcohol am I likely to drink (low, moderate, heavy)?
- Are my drinks mostly no/low carb or carb-containing?
- What therapy am I using (MDI, pump, AID), and how easy is it to reduce insulin safely?
- What’s my glucose doing right now (level + trend), and what insulin is still active?
- What is my overnight plan if I sleep through alarms or symptoms?
Drink categories: carb versus no carb
This is the simplest useful split for glucose management:
- No/low-carb drinks tend to have minimal immediate glucose rise but can carry higher delayed hypo risk later.
- Carb-containing drinks can push glucose up initially, then still create a delayed fall later. This creates a common trap: over-correcting the initial rise and then going low overnight.
John chooses drinks that make glucose management simpler (white wine with soda or spirits with diet mixers). In lived experience, “big nights” can mean large unit totals — and that’s where people often report needing substantial insulin reductions and tighter safety planning. That is not a recommendation; it’s a pattern to respect.
| Drink | Units per drink | Carbs (g) |
|---|---|---|
| Vodka + diet mixer | 1–2 | 0 |
| Gin + slimline tonic | 1–2 | 0 |
| White wine (dry) | ~2 | ~1–2 |
| Red wine | ~2 | ~1–2 |
| Tequila / neat spirits | ~1 | 0 |
| White wine spritzer | ~1.5–2 | ~2 |
Carb-containing drinks can be harder because they create a two-phase problem: early hyperglycaemia risk, later hypoglycaemia risk. If you run an AID system, be aware that automatic corrections can stack insulin when you would actually prefer a gentler response overnight.
| Drink | Units per drink | Carbs (g) |
| Pint of beer | 2–3 | 10–15 |
| Cider (dry) | 2–3 | 15–20 |
| Cider (fruity/sweet) | 2–3 | 30–40 |
| Alcopops / ready-mix | ~1.5–2 | 25–40 |
| Sugary cocktails | 1.5–2.5 | 20–40+ |
| Mixed shots + energy drink | 1–2 | 15–30 |
Insulin therapy considerations (MDI, pump, AID)
This section is not a dosing guide. Instead, here are the common control levers people discuss with their clinical teams, and typical adjsutment ranges.
On MDI (multiple daily injections):
- Primary lever: the background insulin decision (you can’t “turn basal down” later the same way as a pump). typical reductions are 25-75% on the night of drinking, and depends on drinking duration and intensity.
- Bolus: For carb-containing drinks and food, use 0-50% of usual bolus dose. Start low and go slow.
- Practical implication: big alcohol nights can be higher risk on MDI because you may need earlier planning.
- Clinical discussion: how to safely reduce overnight hypo risk without drifting into sustained hyperglycaemia or ketone risk.
On pump therapy:
- Primary lever: temporary basal reductions (and when to start them). Typical reductions of -25% to -75% before drinking begins until the morning.
- Bolus: For carb-containing drinks and food, use 0-50% of usual bolus dose. Start low and go slow.
- Practical implication: pumps allow faster response to trends, but intoxication can impair judgement and lead to over-adjustment.
- Clinical discussion: safe boundaries for temp basal changes and when to avoid correction boluses.
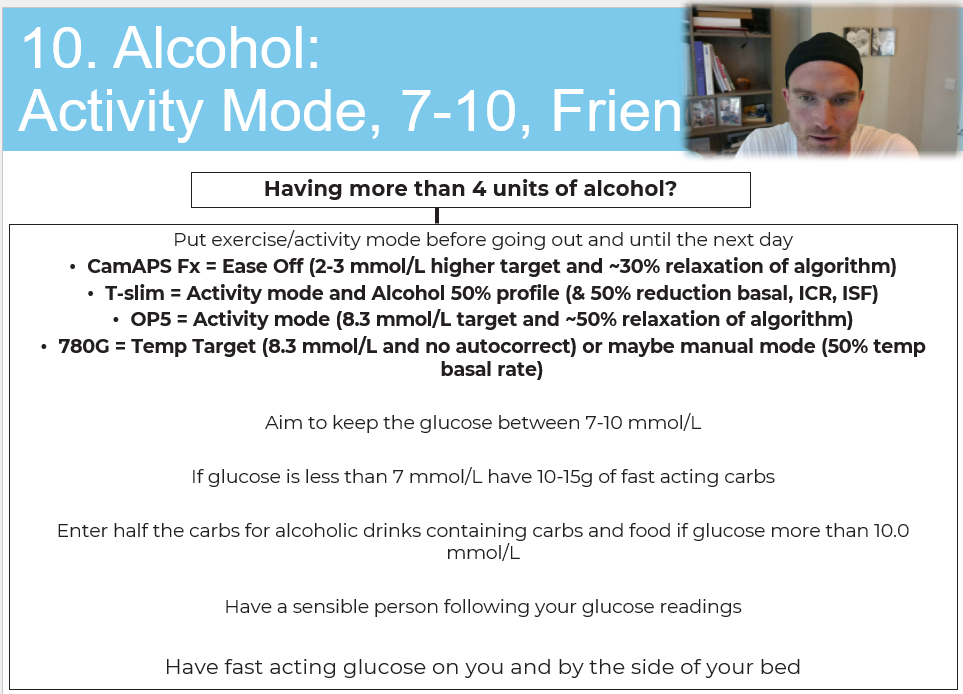
On AID / hybrid closed loop systems:
- Primary levers: activity mode / higher targets, and awareness of automated corrections.
- Activity Mode: Turn on before drinking and keep active overnight
- Bolus: For carb-containing drinks and food, use 0-50% of usual bolus dose. Start low and go slow
- Automatic corrections: carb-heavy drinks or late food can trigger autocorrections that increase delayed hypo risk later.
- Clinical discussion: how to use higher targets safely overnight and when to accept a “slightly higher but safe” range to reduce severe hypo risk.
- Manual mode / Open Loop: May require manual mode or open loop therpay if hypoglycaemia becomomes an issue.Typically manual mode with 50% usual basal is a starting point
If you want AID-specific optimisation, this is relevant: Top tips to optimise time in range with AID systems.
Late-night hunger and the insulin trap
Late-night hunger is common. Alcohol can increase appetite and reduce restraint. This is where many people misjudge insulin: they see a high, eat a lot, or correct aggressively — and then go low later when the liver is still impaired and sleep blunts alarms and symptoms.
Harm-reduction rule from lived experience: when judgement is impaired, bias towards avoiding severe hypoglycaemia. That often means accepting that glucose may run a bit higher overnight, while keeping monitoring and safety tight.
The table below is not a prescription — it’s an illustration of how people think in patterns (glucose band → carb decision → insulin caution).
| Glucose level | Typical carb decision pattern | Insulin caution pattern |
| <7 mmol/L (<126 mg/dL) | Eat carbohydrate | Avoid adding insulin when intoxicated |
| 7–10 mmol/L (126–180) | Small snack or hold | Be cautious with correction |
| >10 mmol/L (>180 mg/dL) | Often avoid extra carbs unless needed | Avoid aggressive corrections |
| If eating more than planned | Consider smaller portions, slower eating | If insulin is used at all, keep it conservative and clinically discussed |
Emergency planning: medical ID, glucagon, and friends
If alcohol is in the mix, plan for the scenario where you cannot self-rescue. That’s not pessimism — it’s competence.
- Wear medical ID.
- Tell at least one person you trust that you have T1D and what a severe hypo can look like.
- Carry fast-acting glucose.
- Consider CGM sharing and location sharing when possible. Best tips for using CGM
- Know that glucagon may be less reliable after heavier drinking because the liver may not respond as expected. [2]
Festival & big night out kit list
| Festival & big night out kit list |
|---|
| Glucose tablets |
| Fingerprick meter (CGM isn’t enough) |
| Backup CGM sensor (or two pre-inserted) |
| Medical ID bracelet/card |
| Fast-acting carbs (juice, sweets) |
| Water bottle |
| Insulin pens/syringes (even if on a pump) |
| Portable battery pack |
| Phone with CGM + location sharing on |
| Anti-nausea tablets |
| Spare cannulas |
You can download the PDF version of the alcohol tips graphic here: Alcohol tips PDF

Practical
This is the minimum viable plan people use when they want to reduce risk without pretending they can control everything.
- Before: eat something; check trend + insulin on board; decide your “ceiling” for the night (roughly how heavy this might get).
- During: avoid stacking corrections; keep glucose visible; hydrate; tell someone you trust.
- Carbs: know whether your drinks are low-carb or carb-heavy; anticipate the two-phase pattern (up then down).
- Overnight: assume you may sleep through symptoms; use CGM sharing/alarms where possible; accept slightly higher targets if needed to avoid severe hypos (especially with AID).
- Morning after: treat it as still “in play”; monitor longer than you think; delayed hypos are common. [1] [3]
What’s next
Move to the next parts of the Partying with T1D system.
Navigation
- Part 1: Partying with T1D (Hub + Intro)
- Part 2: Alcohol and T1D
- Part 3: Stimulants and T1D
- Part 4: Cannabis, Ketamine and Hallucinogens
GNL resources
- Episode 25 — Alcohol with T1D with Dr Dessi Zaharieva
- FAQ — Alcohol and T1D
- Download the Alcohol & Type 1 Diabetes FAQ (PDF)
- Hypoglycaemia: recognition and treatment
- Mastering CGM: top tips
- Optimise time in range with AID systems


Brilliant advise! Living with Type 1 myself, so refreshing to hear honest, realistic advice about something we’re not supposed to do! Well done!
I’m not into drugs myself but great to know there is advise out there for people with Type 1 who are or may want to experiment. With over 30 years now in the diabetes club I’ve perfected the art of safe over indulgence with G and slim line T but I didn’t know about the glucagon thing.
Thanks John and keep up the good work 😁
Kate