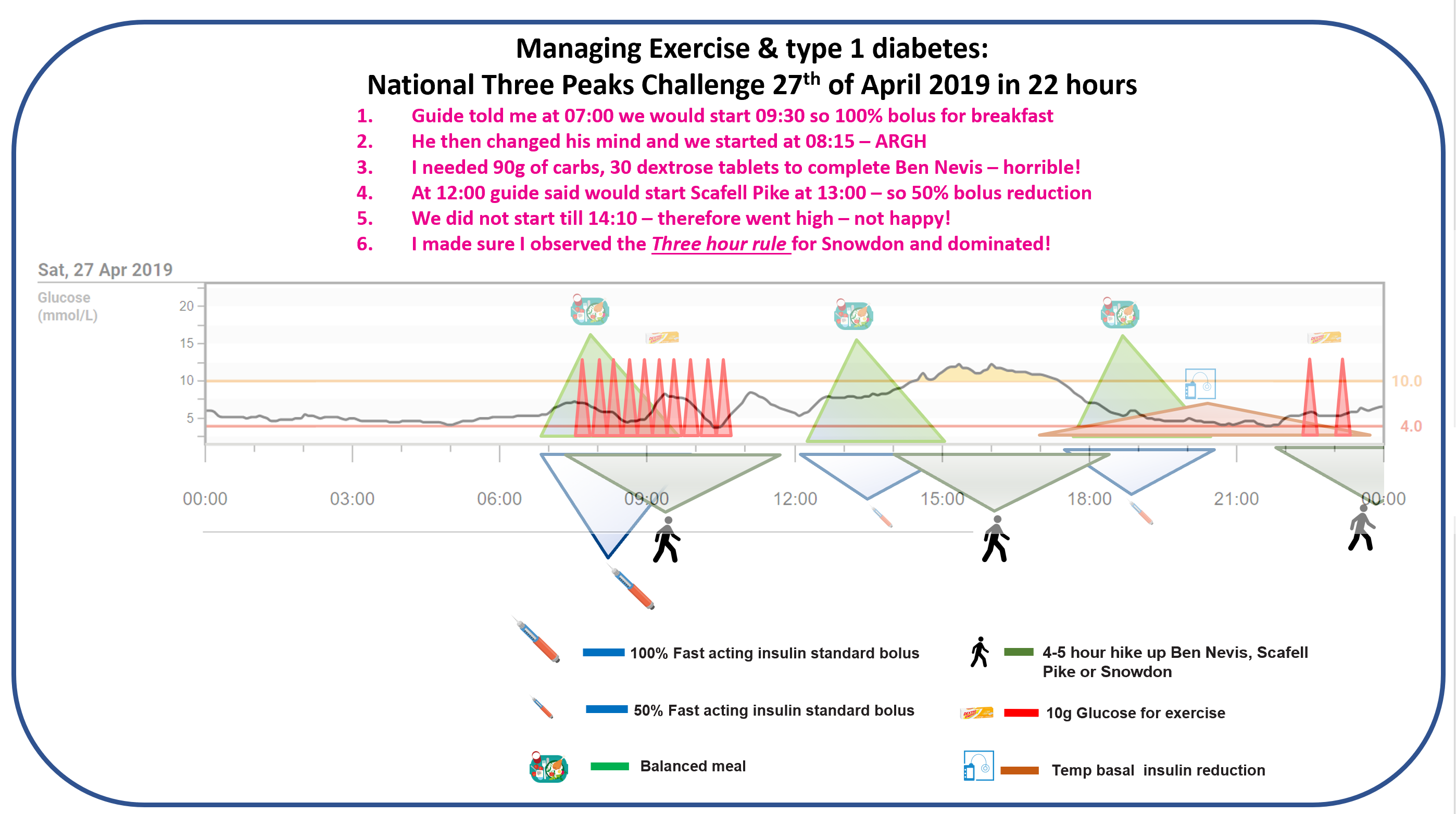
This is the Exercise & Type 1 Diabetes guide. Its purpose is to make exercise predictable enough to manage — without pretending it can ever be perfectly controlled.
For people living with type 1 diabetes, exercise can feel uniquely destabilising. Glucose drops that arrive fast and hard. Spikes that appear late and linger. Sessions that look identical on paper but behave very differently in real life.
The common conclusion is that exercise is “unpredictable”. That conclusion is understandable — and usually wrong.
Exercise does not introduce randomness. It introduces fast, powerful physiology into a system otherwise governed by slow, blunt insulin. When you understand the dominant drivers of glucose change during exercise, patterns start to appear — and with them, control.
This guide is built around heuristics to experiment from. They are grounded in the evidence base and clinical practice, but they require individual tailoring. They are not rigid rules. They are starting points that survive contact with CGM and real life.
Guides and supporting resources in this section:
- Aerobic (endurance) exercise
- Anaerobic (sprinting & lifting) exercise
- Mixed / team sports
- AID systems and exercise
- FAQ: Exercise and Type 1 diabetes
- Podcast episode: Prof. Othmar Moser on exercise and Type 1 diabetes
Major in the majors
If exercise has felt chaotic, start here. Across almost all forms of exercise, glucose behaviour is dominated by a small number of variables.
In order of importance:
- Insulin on board — especially recent bolus insulin
- Starting glucose value
- CGM trend arrows — direction and speed of change
When you prioritise these, exercise stops being mysterious and starts becoming manageable. Most exercise-related hypoglycaemia and volatility can be predicted from these starting conditions.
The core problem exercise creates
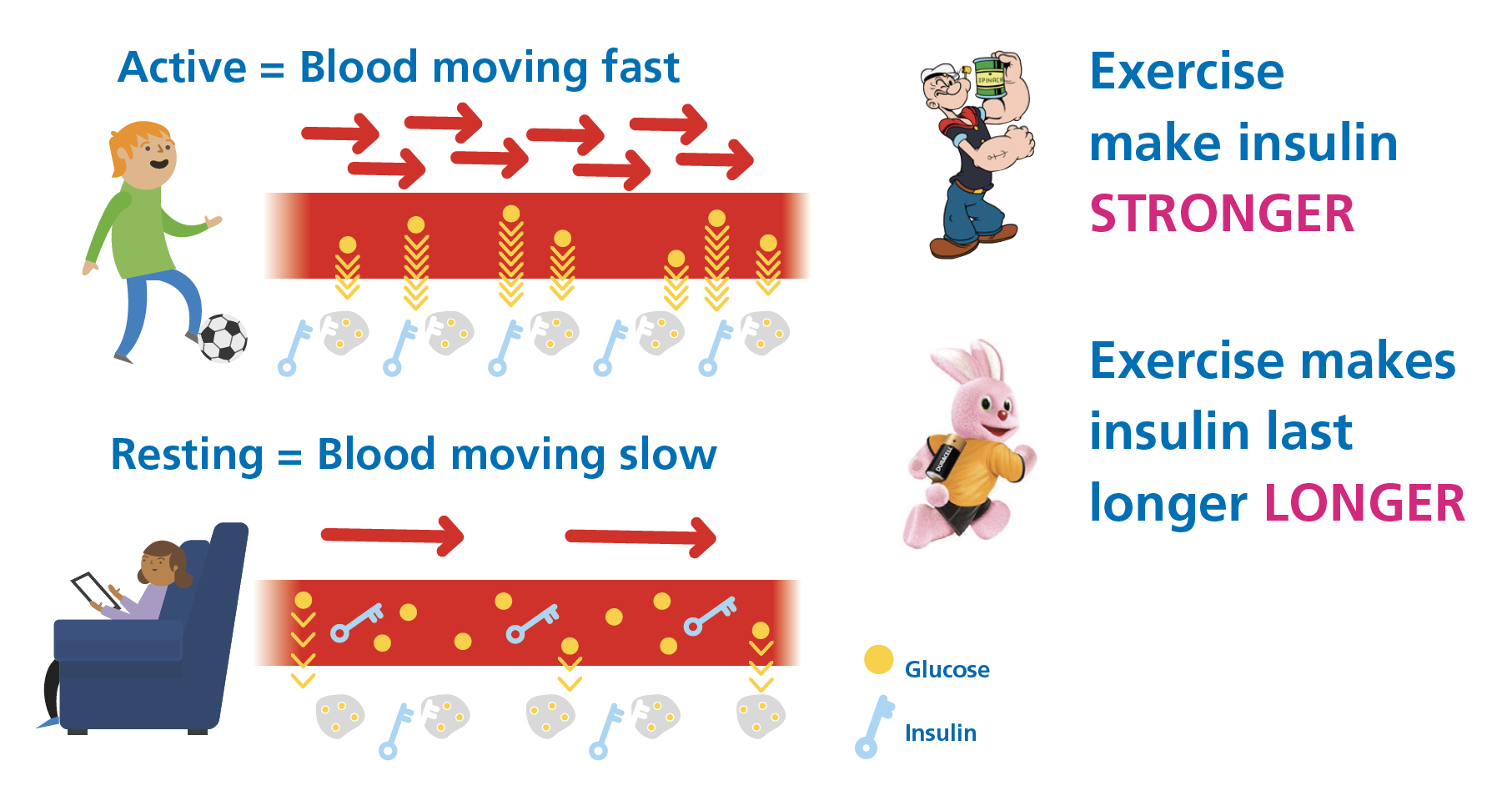
Exercise is hard to manage in type 1 diabetes not because it is dangerous, but because it amplifies insulin action.
Muscle contraction increases glucose uptake. Blood flow accelerates insulin delivery. Counter-regulatory hormones may push glucose out of the liver. These processes act quickly.
Injected or pumped insulin does not.
Exercise hypos are usually insulin problems
Large glucose drops during exercise are rarely caused by exercise itself. They are almost always caused by supercharged insulin action.
Exercise increases blood flow and glucose uptake, amplifying the effect of insulin that is already present. When significant bolus insulin is still active, glucose can fall rapidly. This is physiology doing exactly what it should.
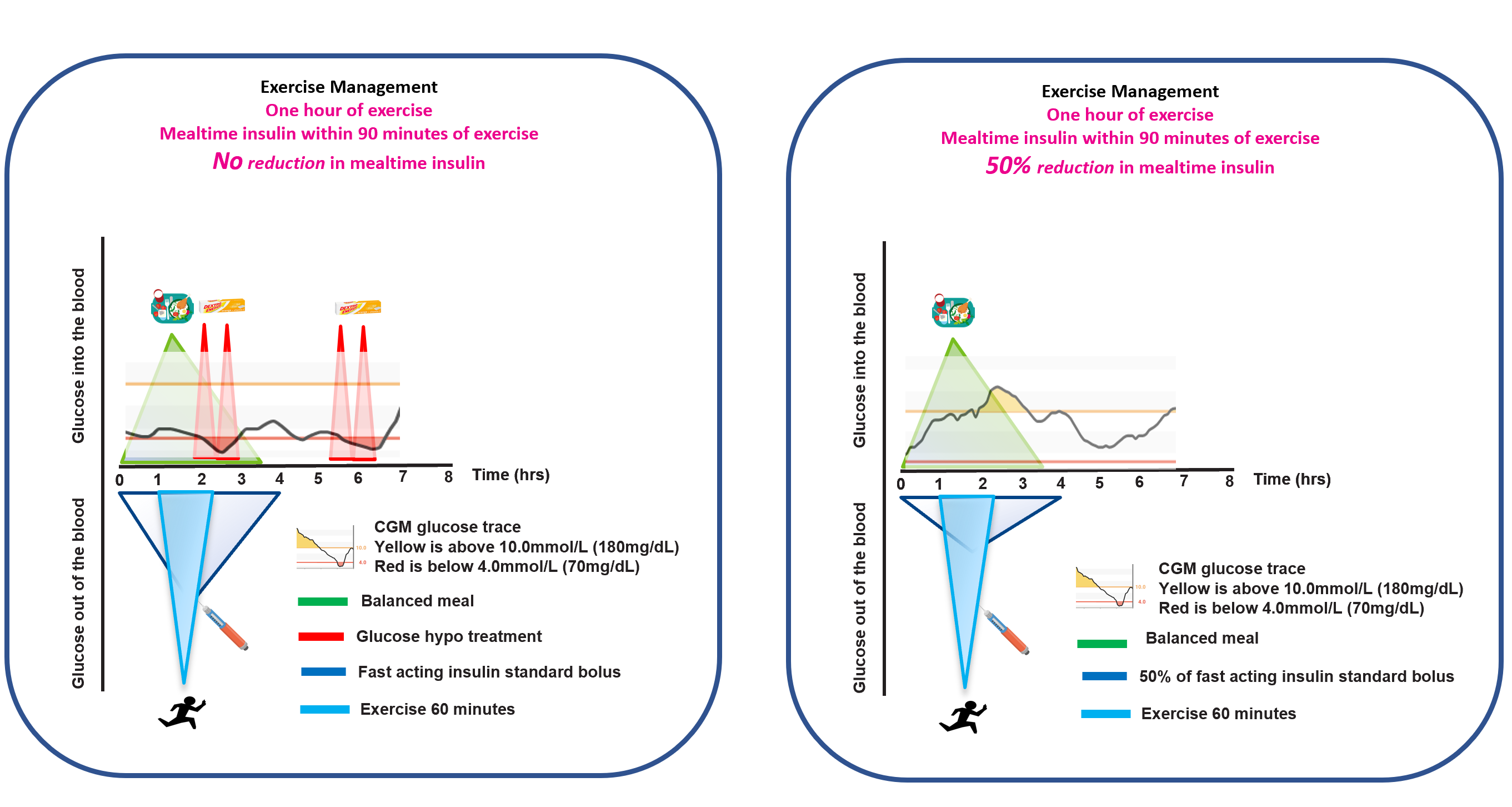
The 90-minute window
If exercise occurs within roughly 90 minutes of a meal bolus, insulin action is often near its peak. In this window, bolus reduction is commonly required to avoid predictable hypoglycaemia.
The Three-Hour Rule
One heuristic simplifies exercise management more than almost any other.
The Three-Hour Rule: when the last bolus was at least three hours before exercise, glucose behaviour is often far more predictable.
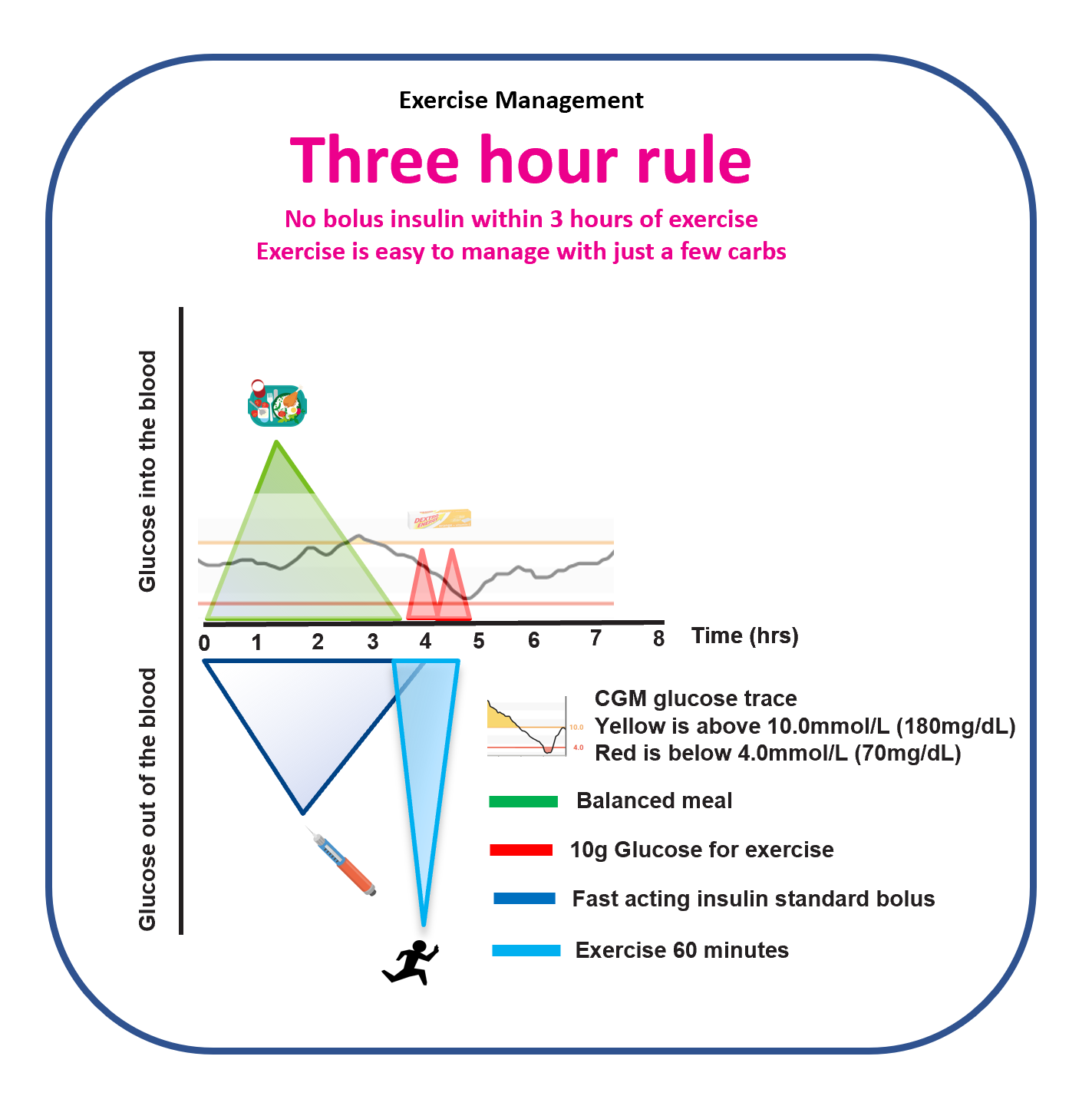
This is not a guarantee — it is an organising principle that often reduces hypos, corrections, and mental load.
Carbohydrate decisions during exercise
Carbohydrate decisions during exercise work best when they are based on both glucose value and trend direction.
- Glucose value
- Trend arrow
Numbers without direction are incomplete information. As a starting heuristic, check before exercise and reassess at least every 30 minutes during activity, using value + trend to decide on carbohydrate intake.
How much?
That’s why we created;
- Dexcom – Exercise Carbohydrate Calculator
- Libre – Exercise Carbohydrate Calculator
- Medtronic – Exercise Carbohydrate Calculator
CGM and AID during exercise
Exercise is one of the times when CGM data becomes less reliable due to lag and artefacts. This is a context where it pays to be cautious about over-trusting CGM.
AID systems do not remove hypoglycaemia risk during exercise. Insulin on board, starting glucose, and trend direction still dominate. In practice, manual mode is often more predictable during exercise because it removes continuous background adjustments.
Where exercise type fits (secondary)
The type of exercise does matter — but it comes after insulin on board, glucose value, and trend direction. This guide discusses exercise types in their own pages once the majors are in place.
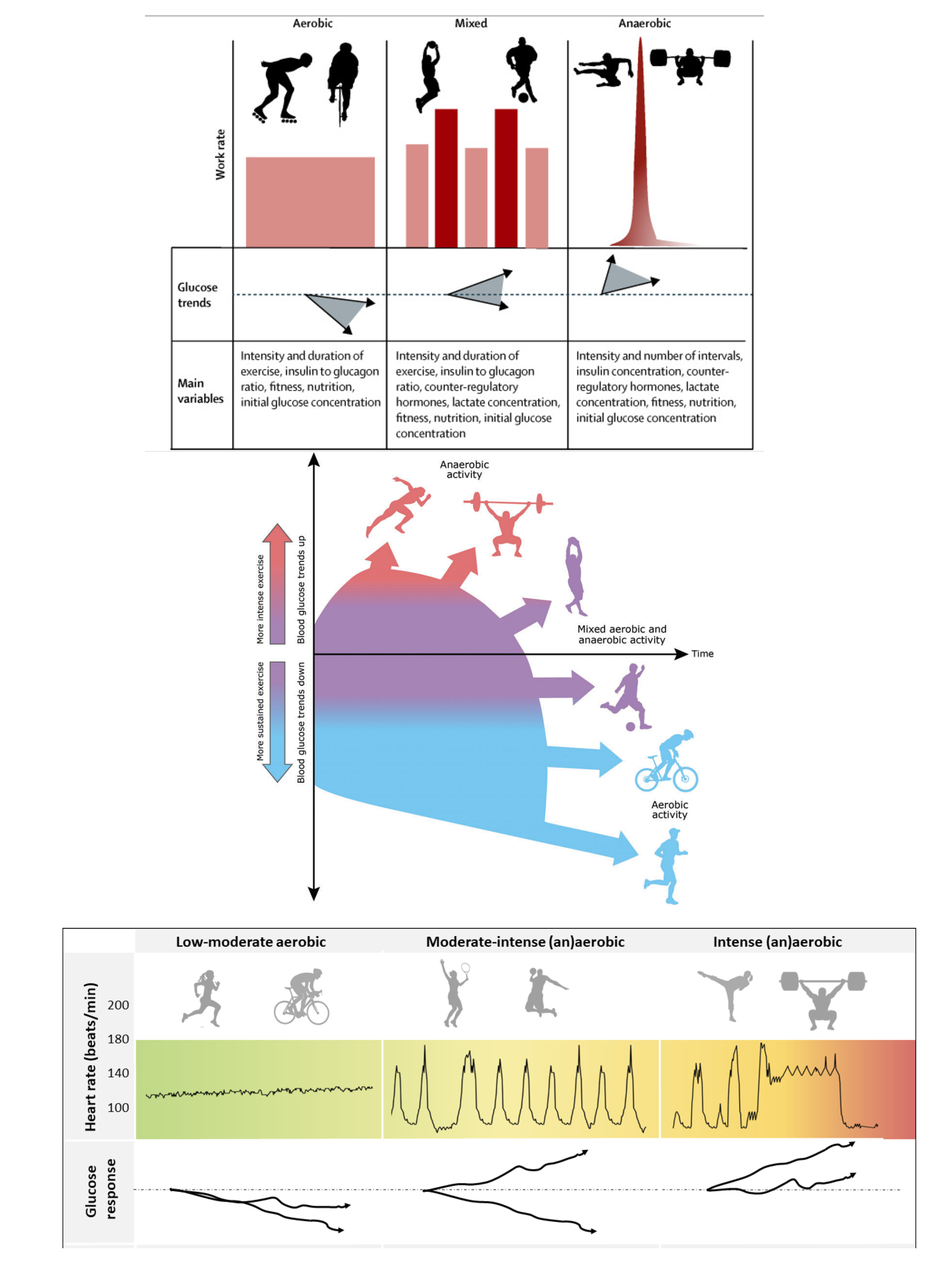
Key mechanisms by exercise type:
- Aerobic (endurance) — tends to lower glucose
- Anaerobic (sprinting & lifting) — often raises glucose
- Mixed / team sports — can rise or fall depending on intensity and insulin on board
What’s next
Start here: Aerobic (Endurance) Exercise
Guides and supporting resources in this section:


I completed your brilliant training on exercise and AID systems, Type 1 DEC (Diabetes Exercise Calculator) Competency and took the post training assessment and scored 10/10 30th April 2025.
I wondered if it would be possible to get hold of the tool please?