Overview
Dynamic Glucose Management is a practical framework for achieving high time-in-range by using fast movers between meals (especially short bursts of activity), instead of relying on insulin corrections alone.
Foundations teaches you how to be safe. This is the section where you learn how to get skilled.
Want to jump straight to the tools? Use these pages in order. They work best as a system.
Prerequisites (non-negotiable): Only continue if you’ve completed — and genuinely understand — the Foundations.
You also need to be using a CGM with alarms. CGM is your teacher and your safety net (and yes, it will occasionally make you furious at 3 a.m.).
The detail
Where this came from
Dynamic Glucose Management has been in development since my diagnosis in 2008 — years of trial and error, repeated failures, and constant tinkering, with my nose in the research trying to understand why glucose behaves in such stubborn, mysterious ways.
My aim is to cut your learning curve to six months or less.
The insight arrived on Christmas Day 2018. The proof came a year later.
Dynamic Glucose Management rests on three pillars:

You’ll need trial and error — with plenty of tinkering — to make the system your own. I’ll guide you, but you’re the one who has to do the work.
Before we go into GAME–SET–MATCH, here’s the story that made the model unavoidable.
Christmas Day 2018: the slow-lane disaster
Grace, you were a year and four months old, and we’d just found out Jude was on the way. Grandma and Grandad were coming down from Bury, the kitchen smelled divine, and the day felt like a proper celebration.
I skipped breakfast, had a bacon sandwich for lunch, then planned to demolish Christmas dinner. I set my high alert at 11.0 mmol/L (200 mg/dL), corrected highs with insulin, and planned to prevent hypos with Coca-Cola.
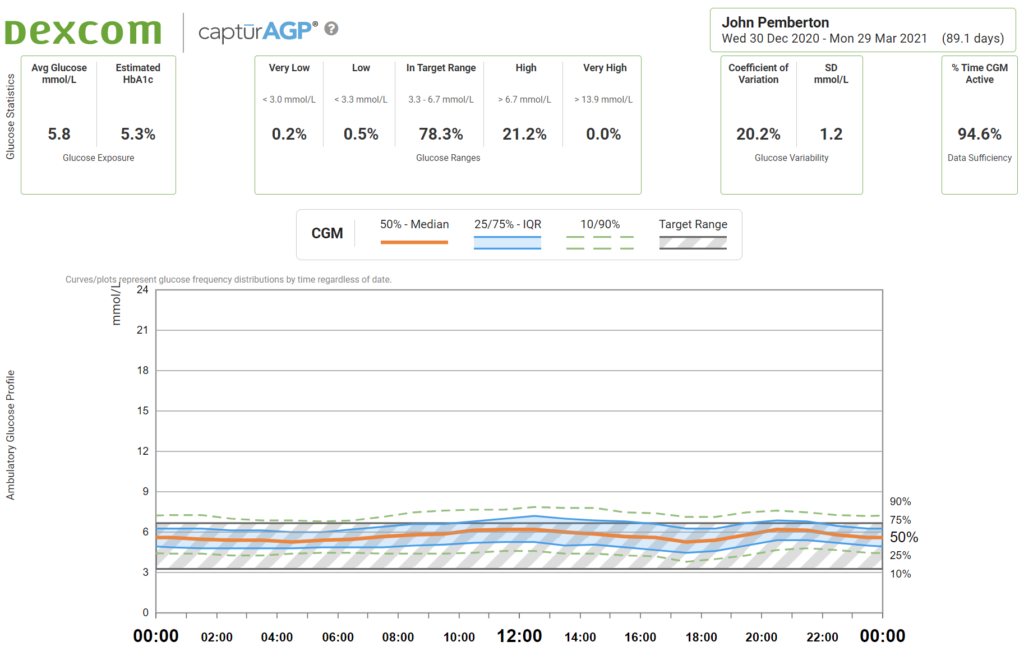
Yes, I know. I’d been duped by the Christmas marketing with Santa chugging the stuff. Also: the man who invented Coca-Cola was called John Pemberton. Destiny? Or irony? Let’s call it a warning.
Here’s how the day played out.
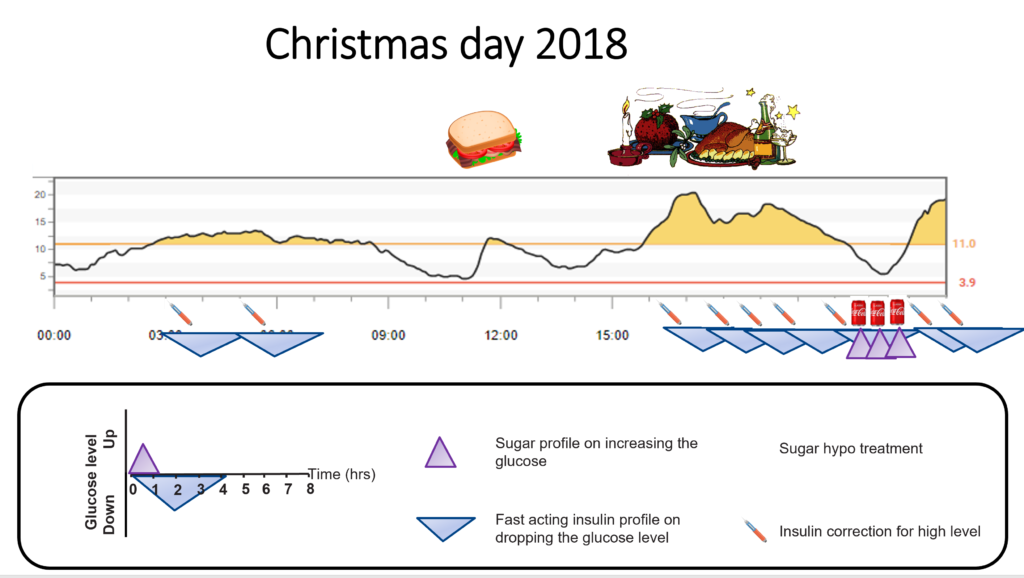
Skipping breakfast and keeping lunch simple worked well. Then all hell broke loose once I attacked Christmas dinner.
I’d done all the “right” things. I weighed and counted carbs within an inch of their life. I delivered insulin 20 minutes before eating. When I added extras, every gram was accounted for.
Then boom: an hour after starting to eat, glucose shot up the mountain. It took five separate correction doses over five hours to get back in range.
Understatement of the year: I was annoyed. Watching glucose climb despite hourly corrections is a special kind of rage.
The meal dose was 10 units (about 200 g carbs). Corrections added another 15 units, taking the total to 25 units.
I knew high-fat meals need extra insulin. I expected more. I did not expect 150% more.
The extra insulin wasn’t the main problem. The problem was the speed: corrections are painfully slow. Fast-acting insulin peaks around 90 minutes and keeps lowering glucose for roughly four hours.
Remember this from Correction insulin?
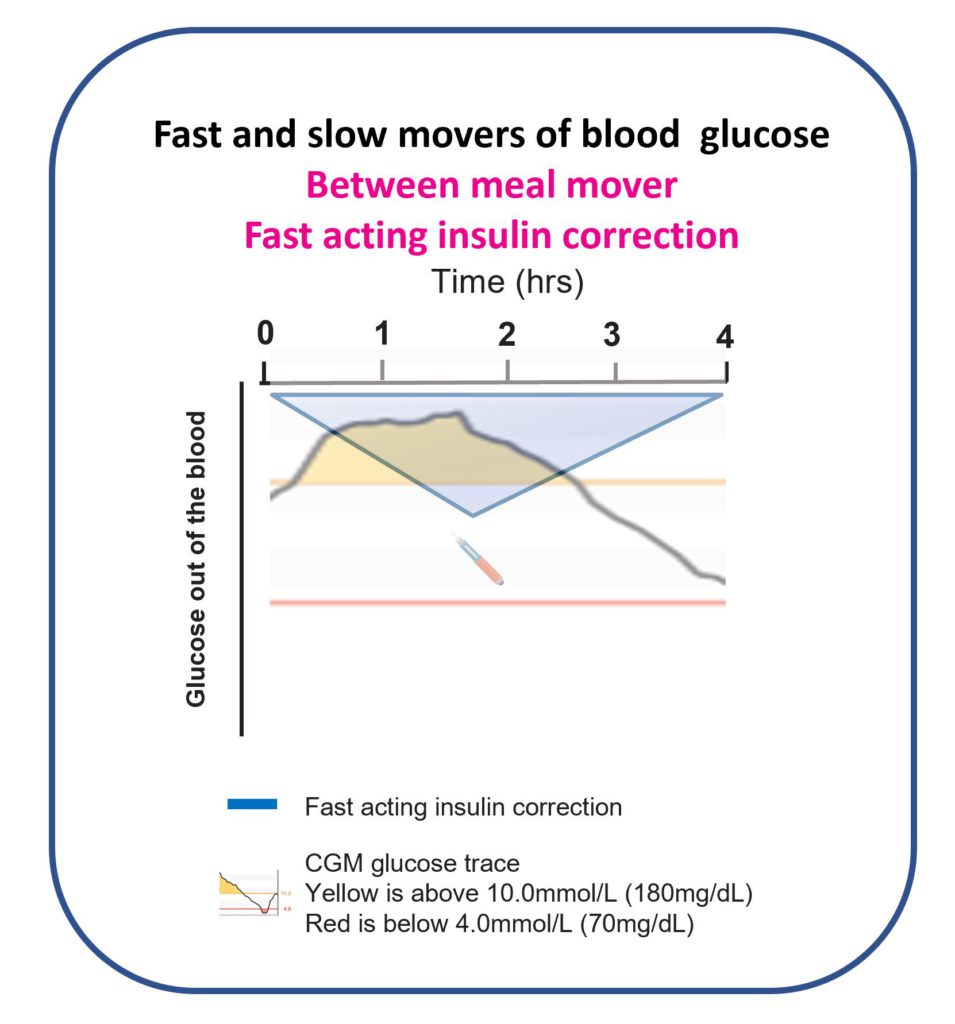
I gave one correction, then another, then another. Four hours later, I could finally see the effect.
By that point, I had so much insulin stacked up that only one thing could happen: glucose nosedived.
I started to panic. I reached for Coca-Cola: 200 ml (about 18 g sugar).
Remember this from Hypoglycaemia?
I waited 20 minutes — still dropping. Another 200 ml. Waited 20 minutes — still falling. A final 200 ml and a stomach like Santa. At last the glucose levelled out… briefly.
Then it headed back up the mountain. With three Cokes back-to-back, I’d stacked glucose in the gut.
I threw in two more corrections before bed, saw no immediate effect, and ended one of the most frustrating diabetes days I’ve ever had.
This was after ten years of living with T1D, working as a Diabetes Dietitian, and thinking I was pretty good at this.
Turns out: The Glucose Never Lies. I wasn’t an expert — not even in my own diabetes.
Back to the drawing board.
The shift: stop living in the slow lane
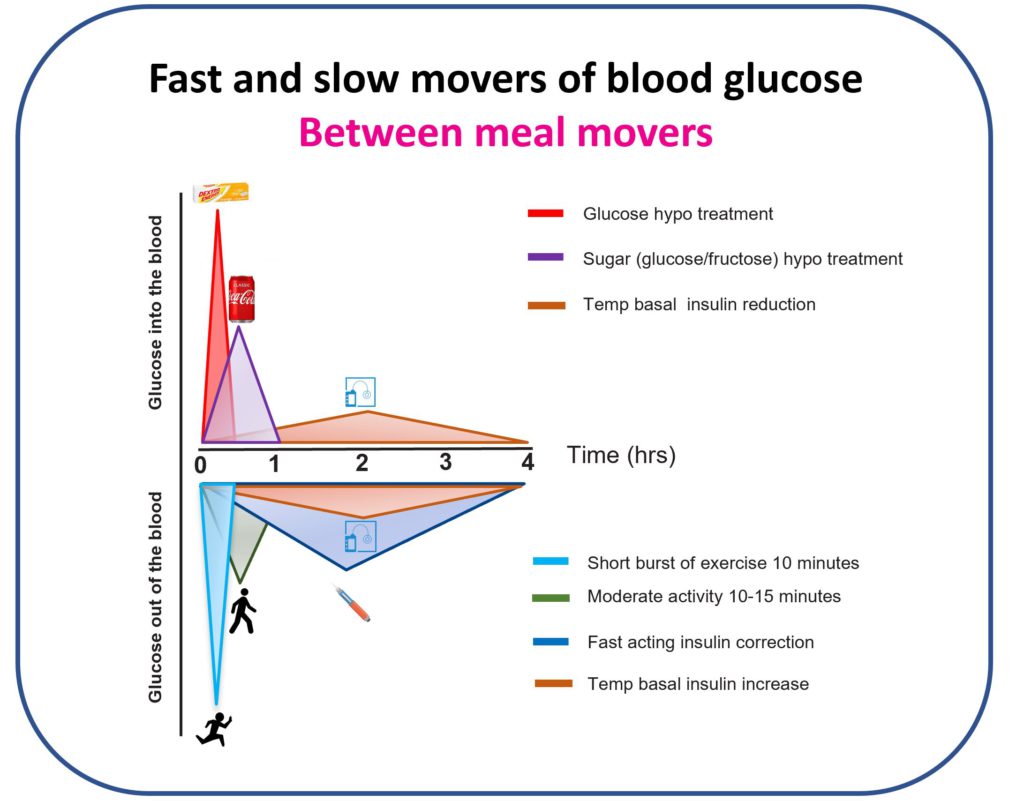
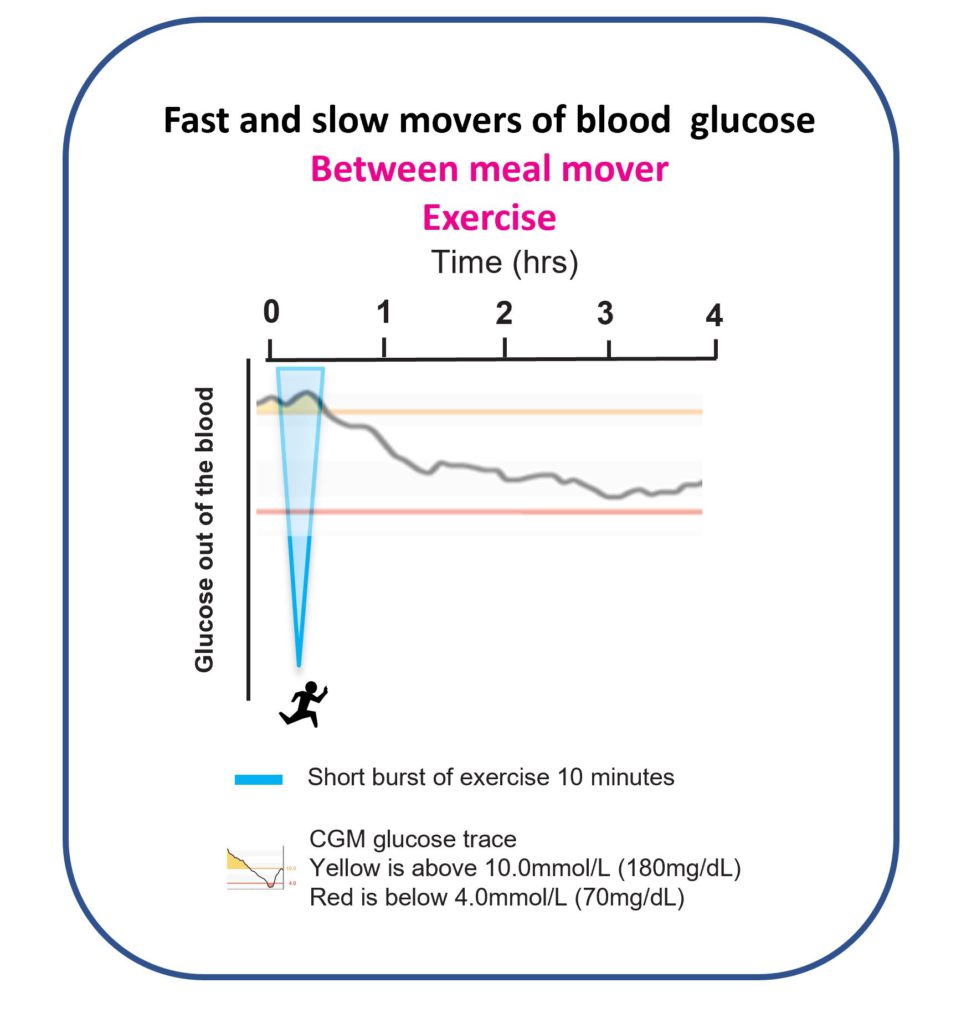
I rebuilt my model of how to think about type 1 diabetes. It became obvious that between meals there are tactics that move glucose very fast, and tactics that are painfully slow.
I’d been prioritising slow movers because that’s what I’d been taught: correcting highs with insulin, preventing/treating lows with temp basals and sugar.
It was time to shift gears and get in the fast lane.
Can you guess what tactics I used on Christmas Day 2019?
Christmas Day 2019: the fast-lane win
Fast forward a year.
Grace, you were two-and-a-bit, and Jude had joined the party. I planned the same food pattern as 2018 — skip breakfast, bacon sandwich lunch, Christmas dinner feast — but this time I committed to fast movers.
I still set the high alert at 11.0 mmol/L (200 mg/dL). But instead of correcting highs with insulin, I used short bursts of exercise.
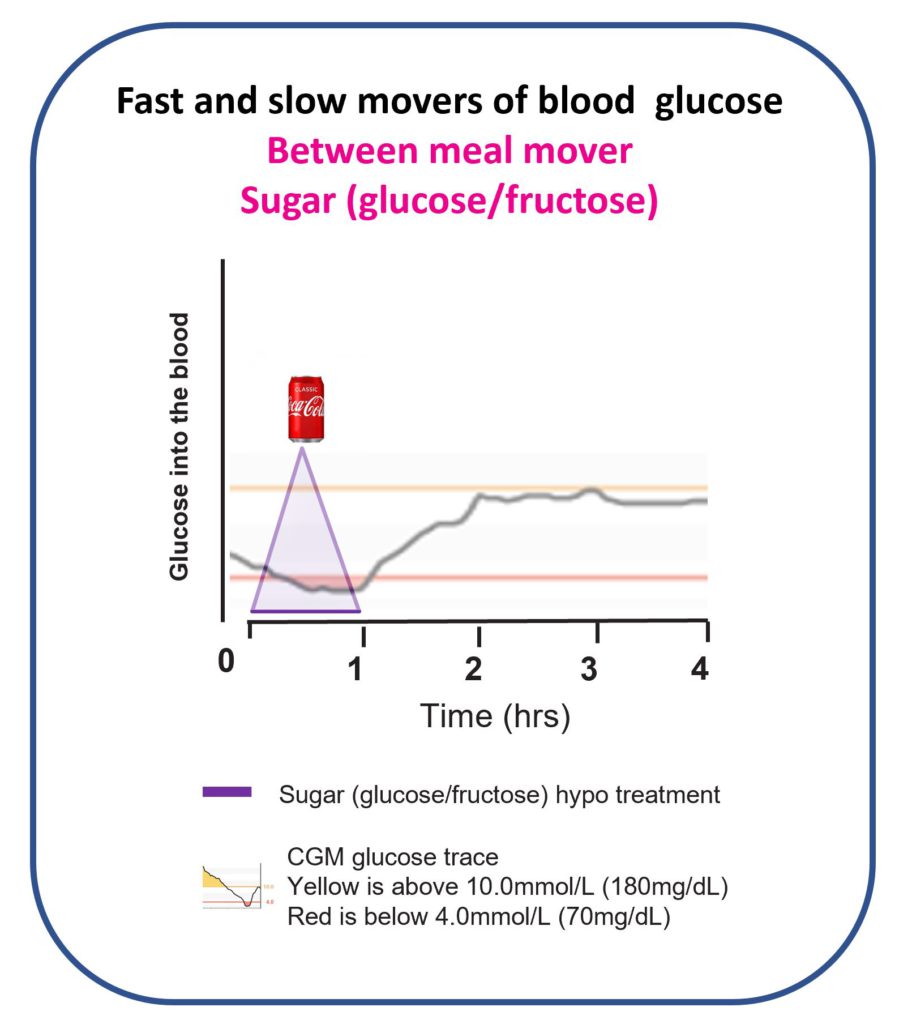
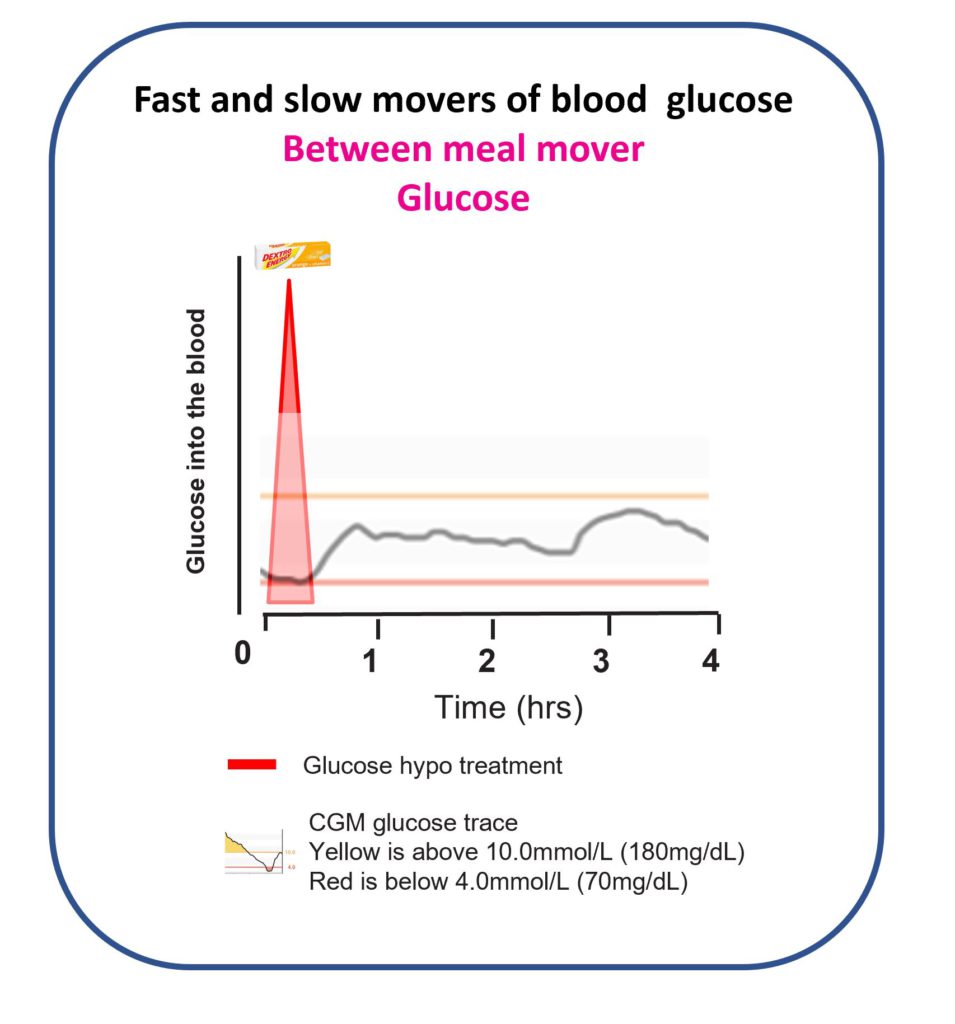
I binned off Coca-Cola and used dextrose tablets for lows. Here’s how the day went.
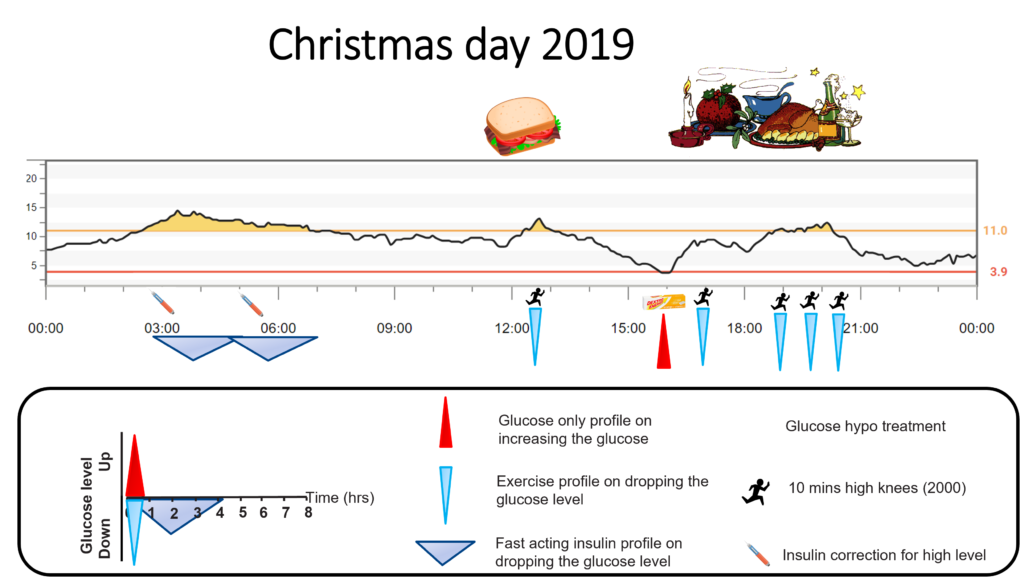
At 39, the overnight excitement still needed two corrections. Even I’m not obsessed enough to do high knees at 3 a.m.
Lunch nudged me up to 11.0 mmol/L. I started jogging on the spot — high knees. Ten minutes later, glucose was dropping and back in target almost immediately. Exactly as the Activity and movement page predicts.
(The Activity Snacking podcast is a must-listen.)
Before dinner, glucose drifted low. My standard prevention dose is ~18 g: six tablets. But the arrow was only gently down, so I used half a treatment: three tablets. Nice controlled bump back to mid-range — fast, clean, no overshoot.
Christmas dinner came and I did not hold back. Roughly the same 10 units (200 g carbs) as 2018.
As glucose started climbing, I did another 10-minute burst of high knees before the alarm even went off. Bosh — the climb got whacked on the head.
Two hours later, pudding + cheese + crackers did their thing. High alarm sounded; knees started pumping again. Over the next 90 minutes I did three bursts, totalling about 10,000 high knees across the day.
Result: in range by bedtime, no insulin stacking, no glucose stacking, safe sleep.
No sane person is doing 50 minutes of high knees every day to manage diabetes. But no sane person is eating Christmas dinner every day either. This was an extreme demo of how fast movers change the game.
That day, the three pillars of Dynamic Glucose Management clicked into place:
Stop highs — GAME — Use short bursts of activity to lower highs between meals, not insulin corrections.
Stay in target — SET — Use meal structure to reduce volatility and make timing work.
Prevent lows — MATCH — Use glucose-only treatments, not sugar, and dose based on context.
What followed was months of real-world trial and error with continual tinkering. By April 2020, the framework was fully formed.
GAME–SET–MATCH
- Stop highs — GAME
- G: Glucose time-in-range desired
- A: Alert on high set according to the desired time in range
- M: Mode of exercise that can be done anywhere
- E: Exercise on high alert based on glucose value and arrow
- Stay in target — SET
- S: Start insulin before eating
- E: Eat three balanced meals
- T: Ten minutes of activity after eating
- Prevent lows — MATCH
- M: Measure weight to calculate hypo treatment
- A: Always use glucose only, not sugar
- T: Try to prevent lows
- C: Change treatment based on glucose value and arrow
- H: Have patience and wait 20 minutes
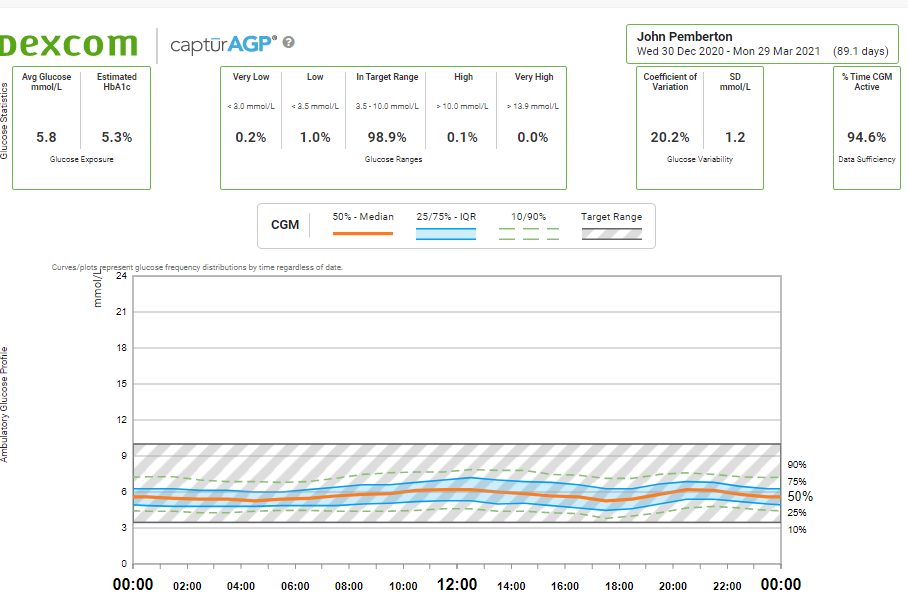
Dynamic Glucose Management took me from ~85% to ~99% time in range (in my own diabetes).
How does this compare with AID systems?
What follows is not a claim about what AID systems can or cannot do in general. It’s a description of what they did — and did not do — in my diabetes.
In my experience, DIY looping, Control-IQ, and the 670G all worked well and typically got me to roughly 85% time in range with ~3% low. Solid control — but not the 99% time in range and ~1% low I was able to achieve using Dynamic Glucose Management during the day.
AID systems do a lot of heavy lifting: they correct highs with more insulin and try to prevent lows by slowing or suspending insulin delivery.
They’re brilliant overnight when liver glucose output is the main variable. But during the day, using only insulin — a slow mover — can’t keep up once food, activity, stress, and chaos enter the room.
In my own data, AID systems typically managed about 50% time in the optimal non-diabetic range (3.3–6.7 mmol/L / 60–120 mg/dL).
Dynamic Glucose Management pushed me to ~80% in that optimal range (in my own data).
For luxurious sleep and near-perfect daytime control, the best setup (for me) is: an AID system overnight, plus Dynamic Glucose Management during the day.
Nothing here comes for free. Dynamic Glucose Management takes time, attention, and a bit of obsession. Some people will love that. Some won’t. Both are fine — it’s your diabetes, your life.
The only thing that can beat this level of control is severe carbohydrate restriction. I’ve explored that too — see the 120-day carbohydrate experiment.
“There is no need to severely restrict carbohydrates to achieve near-perfect control if you use Dynamic Glucose Management.”
The beauty is you don’t need keto or ultra-low carb. You just need to be willing to use fast movers between meals.
What about children and young people?
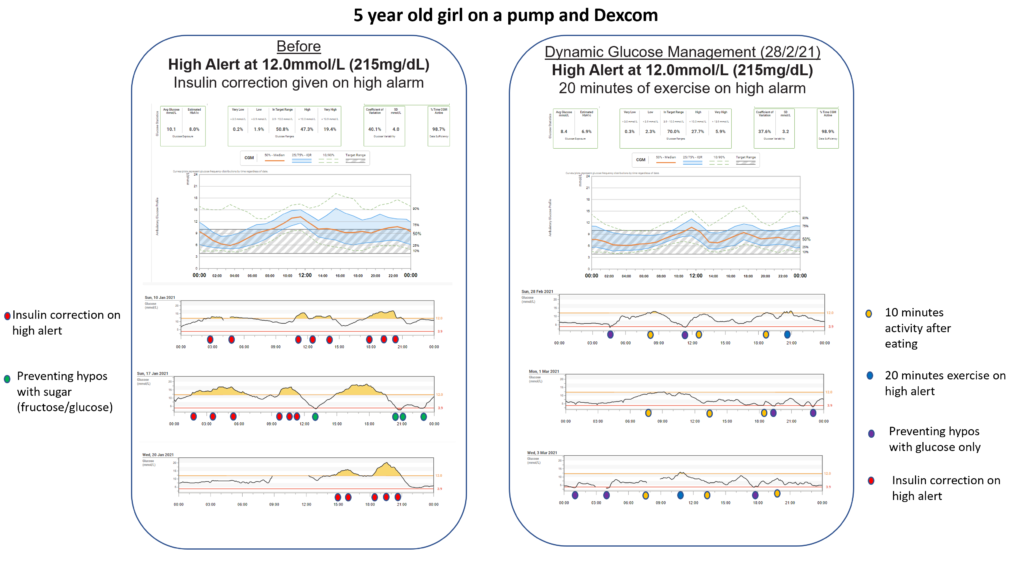
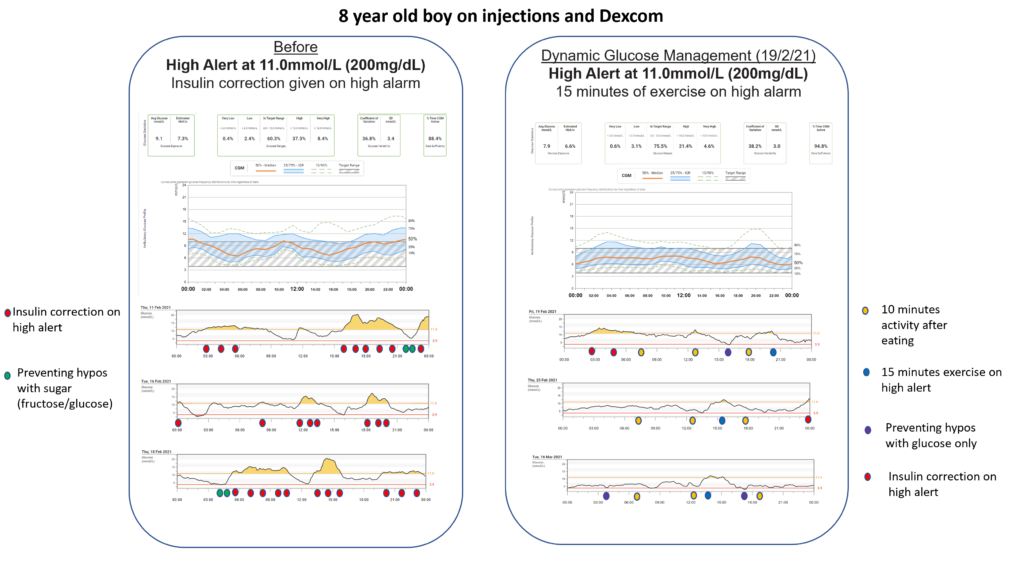
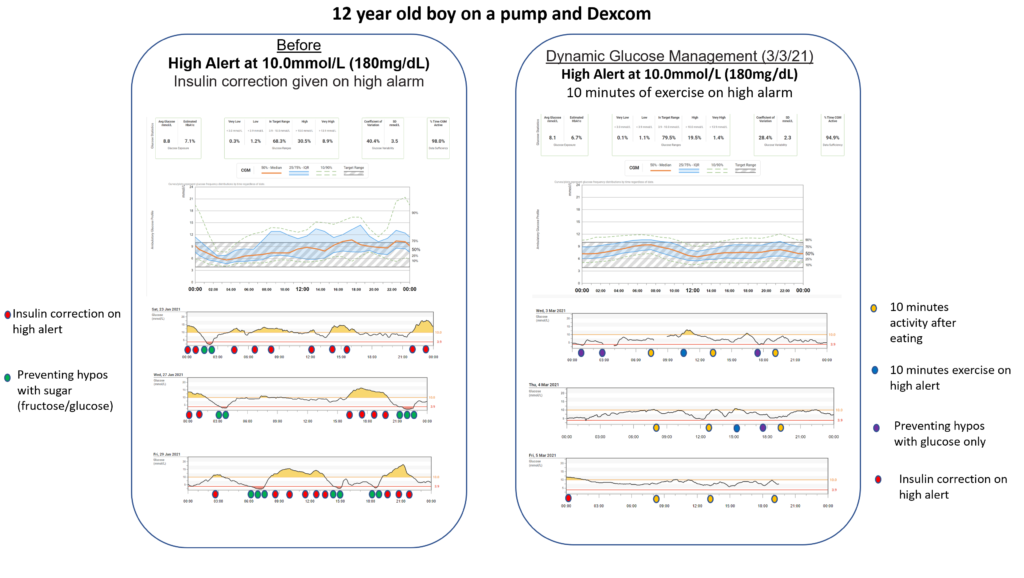
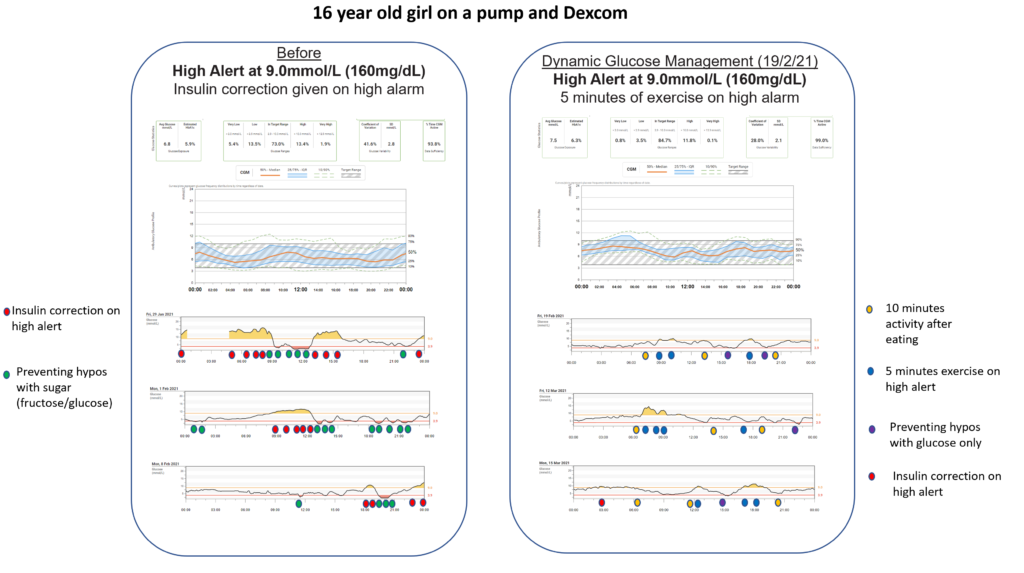
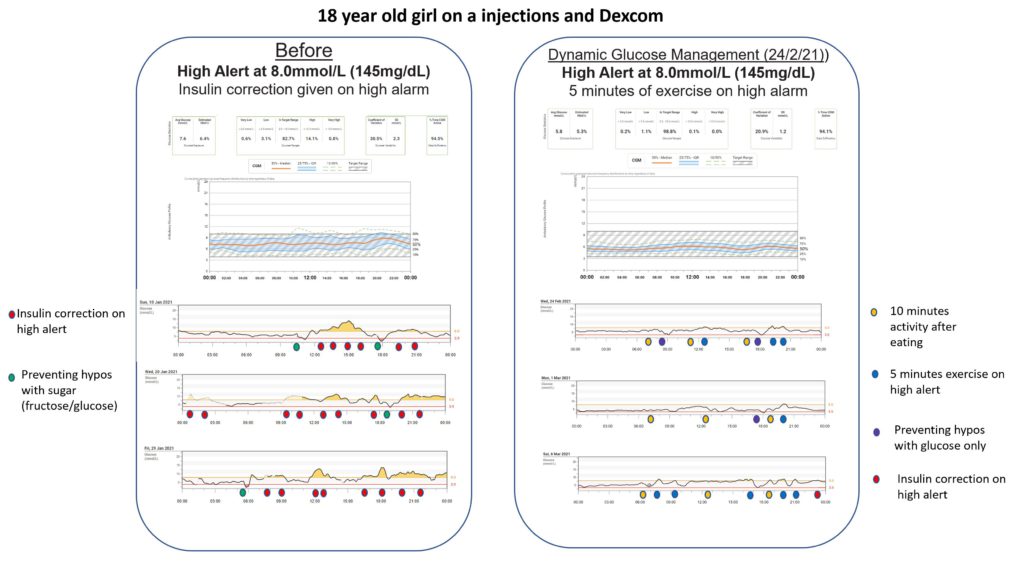
I created a CGM structured-education programme that teaches Dynamic Glucose Management to children, young people, and their families. We introduced it at Birmingham Children’s Hospital and published the first fifty educated (broken down in the Research section).
Using Dynamic Glucose Management stopped problematic hypoglycaemia and increased time in range by ~10% on average.
Those who used it most consistently achieved the highest time in range: roughly 70–90%.
In our audit of the first hundred educated, the strongest drivers of high time in range were: short bursts of activity to correct highs, adjusting pre-meal insulin timing based on glucose and arrows, and preventing lows with glucose (not sugar).
What’s next
The next step is to work through the pillars in order. Don’t jump ahead. Put the reps in.

