This is the Under-5s Guide for type 1 diabetes
It teaches you how to use simple structure + targeted insulin strategy to improve glucose stability in children diagnosed under the age of five — alongside CGM and AID systems, not instead of them.
This age group is uniquely hard because eating is unpredictable, insulin doses are tiny, and hormone patterns are extreme. The goal is not “keeping up”. The goal is repeatable stability that protects health and development over the long run. [1–2]
Overview
Children diagnosed under five face a longer lifetime exposure to glucose variability. Earlier onset is associated with higher long-term risk, including cardiovascular outcomes. [1] There is also evidence linking persistent hyperglycaemia in early childhood with effects on the developing brain. [2]
The practical target is over 70% time in range (3.9–10 mmol/L), ideally over 50% time in tight range (3.9–7.8 mmol/L), and an HbA1c around 6.5% (48 mmol/mol), where safely achievable. [3]
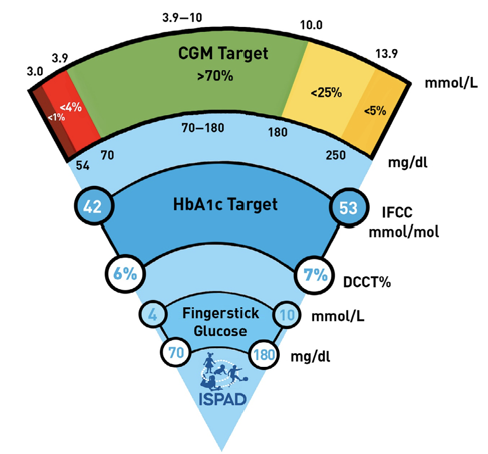
CGM gives visibility, but real-world outcomes show many children still sit around ~54% TIR early after CGM adoption. [4] Even with Automated Insulin Delivery (AID) systems, median TIRs in this age group are often around the 60–65% range in published cohorts. [5]
This is not because parents are failing. It’s because the system has to manage: (1) fast-changing insulin resistance, (2) erratic intake, and (3) very small dosing where tiny errors matter. The solution is a hybrid approach: technology + structure + targeted settings changes.

The detail
Glycaemic targets and the limits of technology
AID systems are helpful, but they are not mind-readers. They struggle most when:
- food intake is variable (toddler behaviour is not “doseable”)
- insulin requirements swing fast (time-of-day hormone effects)
- doses are tiny (small errors have big consequences)
So the strategy is not “trust the algorithm harder”. It’s to make the day more predictable and tune the known danger windows so the system has a chance to perform.
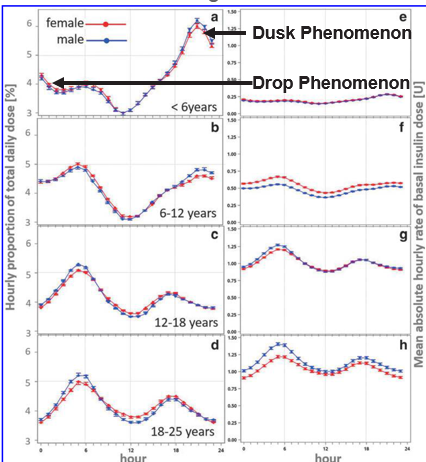
Dusk-Then-Drop phenomenon
One of the most common under-5 patterns is the “Dusk-Then-Drop” phenomenon:
- 17:00–22:00: insulin resistance rises (glucose pushes up)
- 22:00–02:00: resistance drops (risk of overnight lows rises)
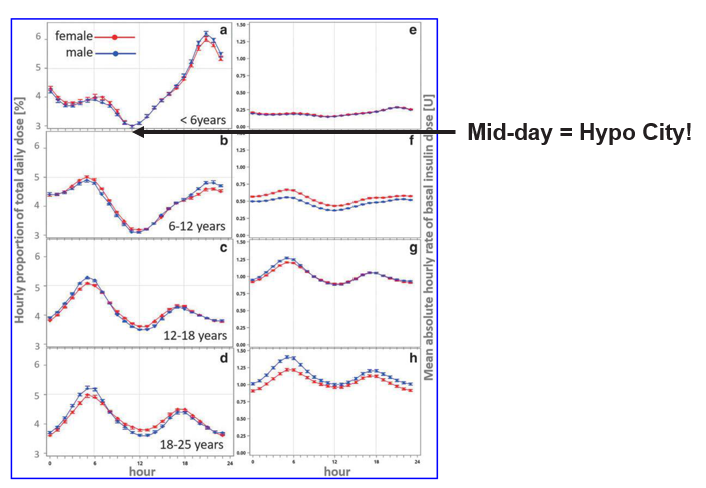
DPV registry data show that children under six have the largest swings in insulin requirement of any paediatric age group, making this time window hard even with AID. [6]
What to do (hybrid approach):
- Lower targets and/or make correction factors more aggressive early evening 17:00–22:00 to blunt the dusk rise.
- Consider a cautious “fake carbs” bolus around 19:00 (small bolus without food) to stop stubborn dusk rises. Increase gradually in 5 g increments until you find the smallest effective dose.
- Then use a higher target and/or weaker correction factors from 22:00–02:00 to reduce overnight lows once resistance drops.
This graphic summarises the AID-specific options:
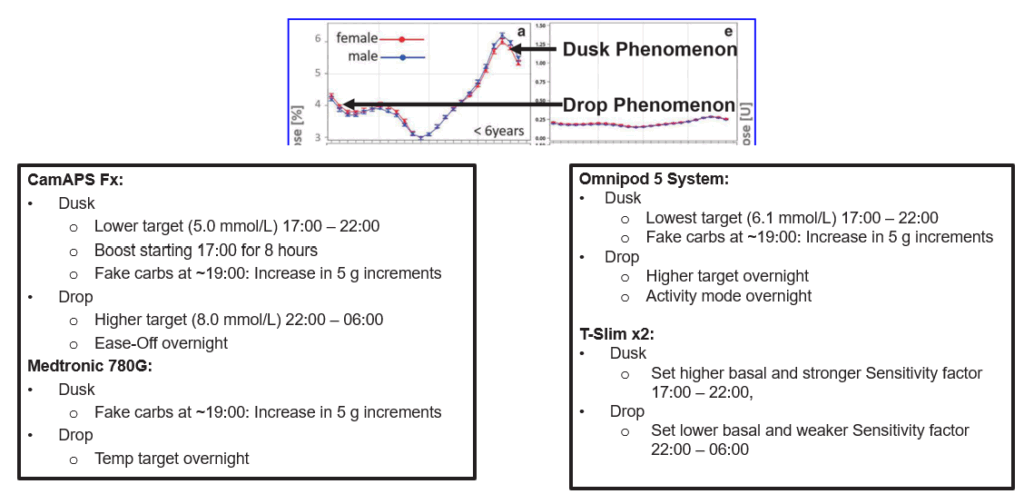
This can be used with pumps or injections. With injections, the smallest increment may be 0.5 units, which can be too large in this age group — so proceed with clinician support and extreme caution.
Here are before-and-afters for different AID systems:
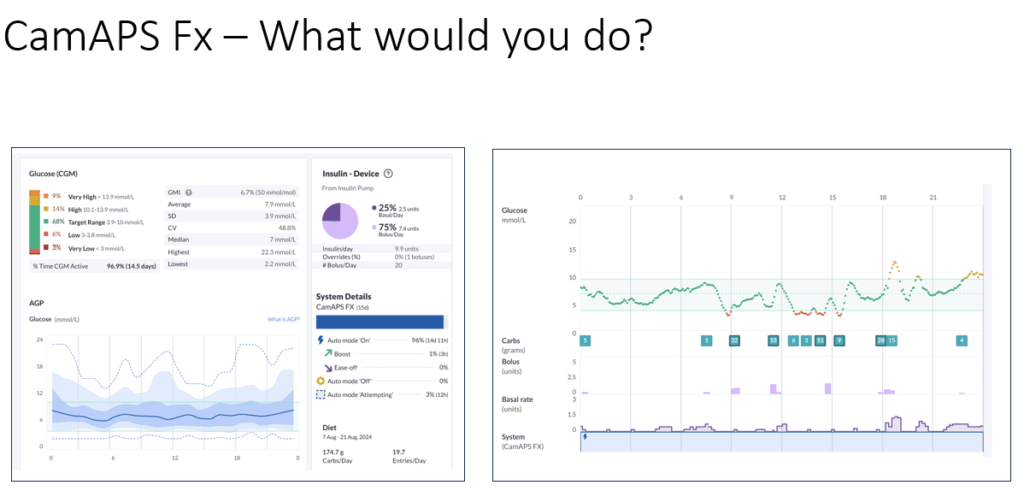
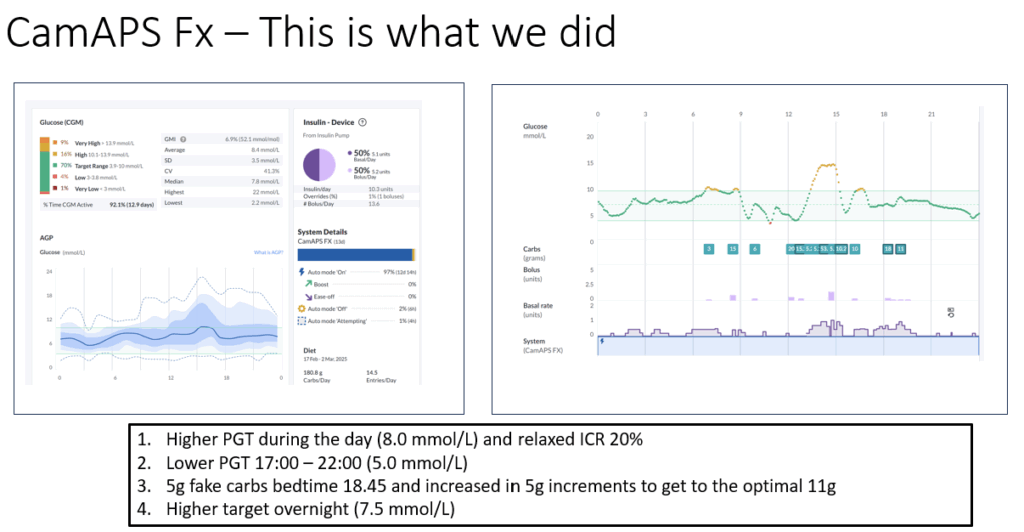
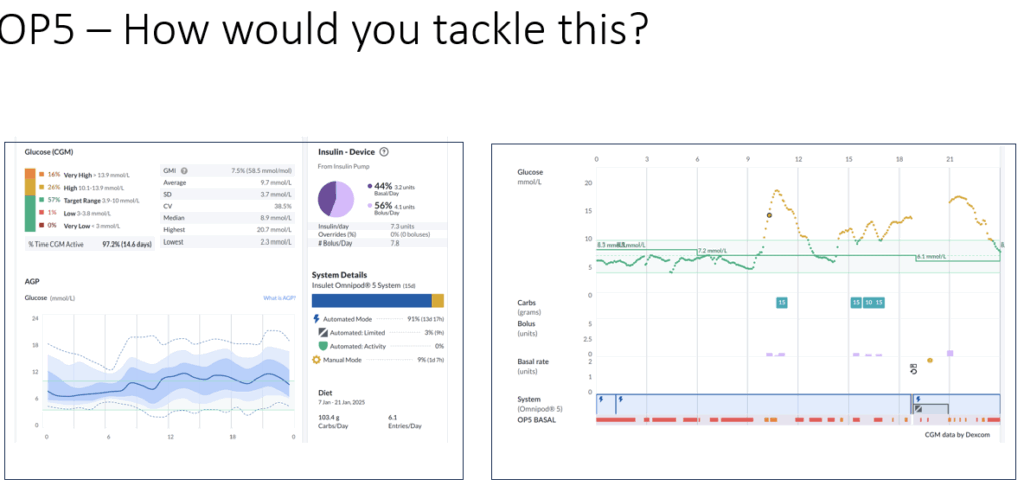
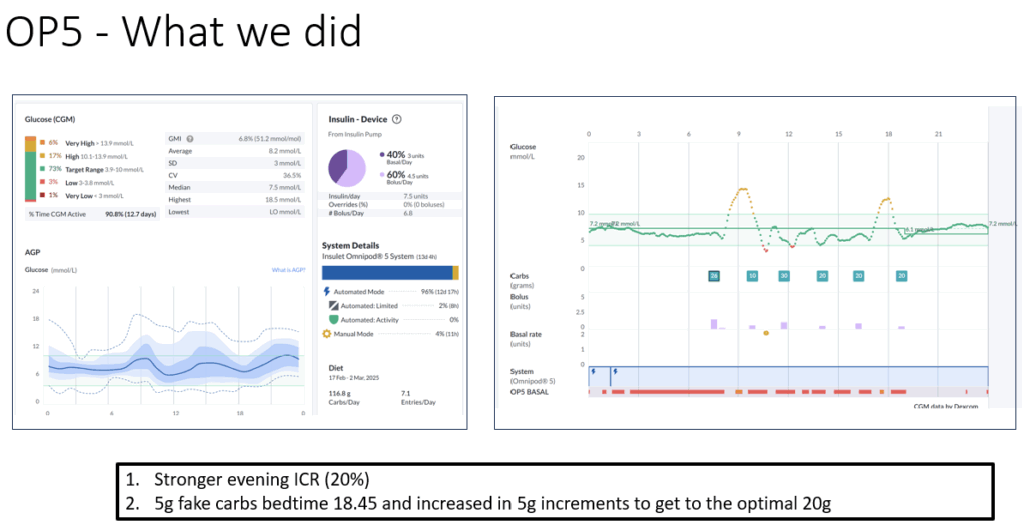
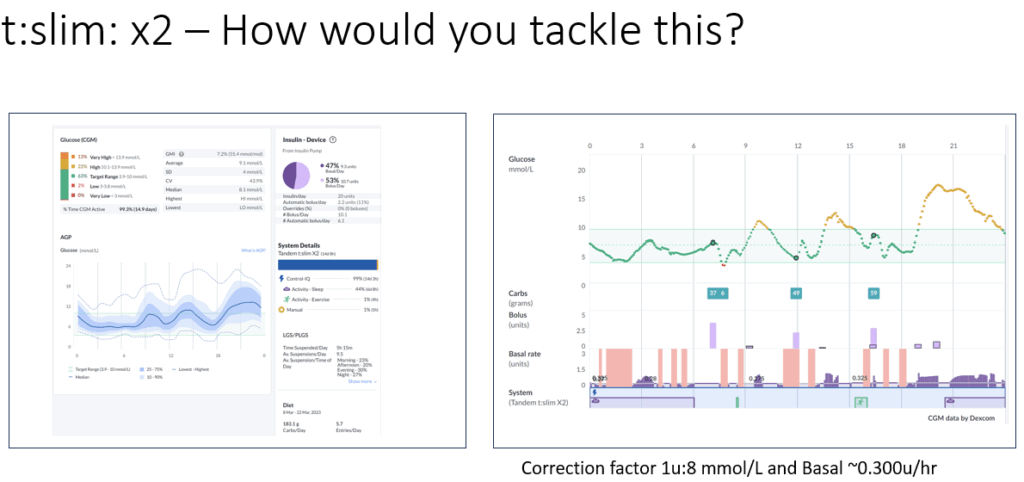
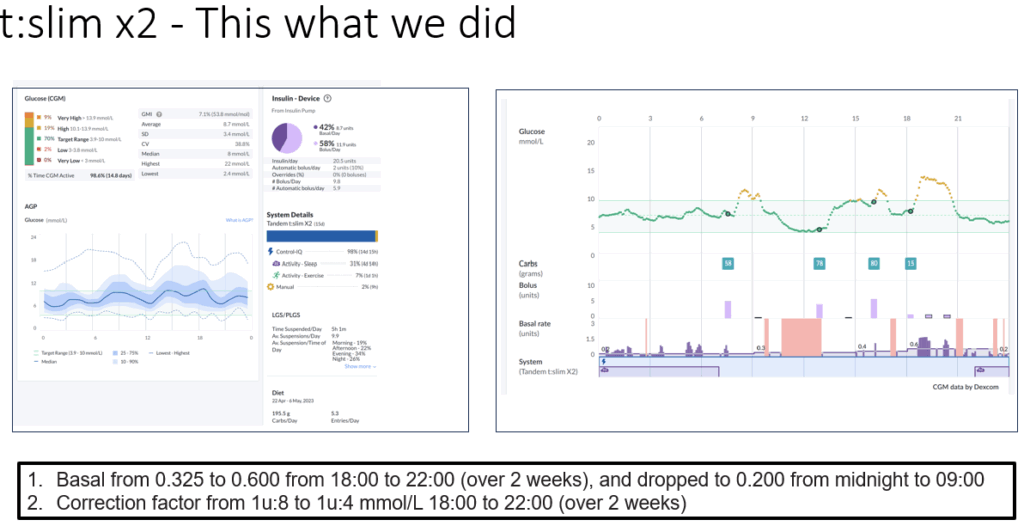
The aim is not zero spikes. The aim is fewer evenings that run away, and fewer nights where insulin is “stuck high” after the dusk phase ends.
Tackling the midday hypo trap
Another common under-5 pattern is hypoglycaemia risk between 11:00 and 14:00. For many children, this is a window of higher insulin sensitivity, especially around and after lunch.
The lever here is often meal-specific insulin-to-carb ratios (ICR). In practice, many under-5s need:
- stronger ratios at breakfast
- weakest ratios at lunch
- moderate ratios in the evening
Starting rules of thumb (based on total daily dose, TDD):
Breakfast ICR: 150 ÷ TDD
Lunch ICR: 250 ÷ TDD
Evening ICR: 200 ÷ TDD
These are starting points, not commandments. The target outcome is simple: fewer midday lows and fewer rebound corrections.
Here are AID system options:
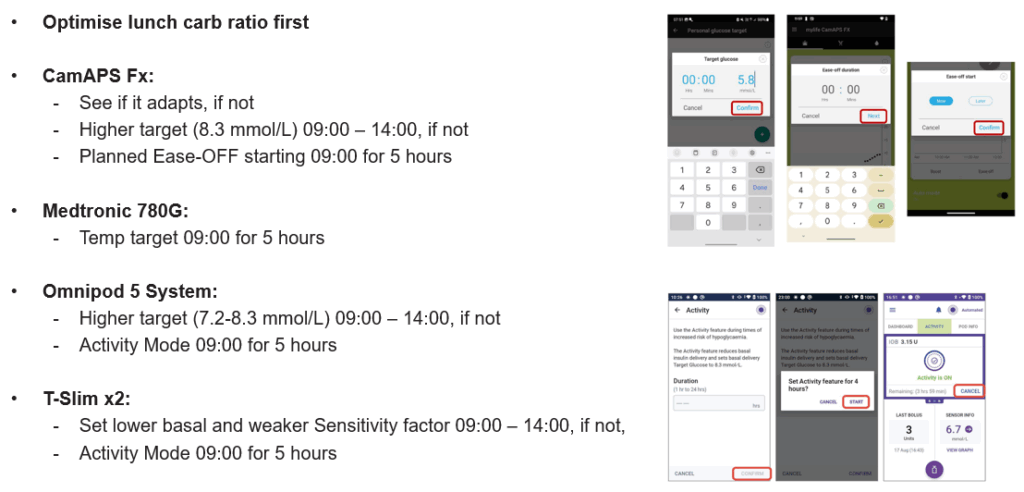
For children with TDD under 5 units, diluted insulin or use of activity mode around meals may be needed to prevent excessive insulin delivery.
Structured meals and confident pre-bolusing
The most powerful lifestyle intervention in this age group is structured eating. Regular family meals at consistent times reduce glucose chaos and make insulin timing more predictable.
Pre-bolusing is central. Aiming for ~15 minutes before eating can meaningfully reduce post-meal spikes. But under-5s are unpredictable, so use a stepped approach:
- Start with 50% of the dose pre-meal
- Then 75% pre-meal
- Work towards 100% pre-meal when confidence and predictability improve
Carbohydrate counting should be as accurate as possible, ideally within 5–7 grams where feasible. Small errors matter more when doses are tiny.
If breakfast is consistently spiky, consider lowering high GI cereals and adding light post-breakfast movement where realistic. The meal insulin guide is worth revisiting regularly.

Parenting with precision: behavioural strategies that work
Under-5 management is not only insulin. Parenting structure reduces glycaemic variability by reducing variability in eating, timing, and stress. The Triple P framework supports routines and insulin timing.
Principles that tend to work in the real world:
- Keep exposing children to new foods and routines, even if they resist at first.
- Use games and challenges to make meals enjoyable.
- Implement small changes gradually.
- Create routines: same time, same place, for meals and insulin.
- Model behaviour: eat as a family, minimise screens at the table.
- Avoid force; instead, offer choices.
- Use positive reinforcement (stickers/charts) to build cooperation over time.
- Plan the day to reduce decision fatigue.
- Focus on long-term consistency rather than daily perfection.
The point is not “perfect parenting”. The point is a calmer, more predictable day so insulin strategies and AID systems have a fair chance to work.
Nutrition and insulin: getting the basics right
Do not lose the basics while chasing numbers. Use Schofield equations (or equivalent) to estimate energy/protein needs, and aim for balanced meals that support growth. A practical baseline is ~40–50% of intake as carbohydrate, adjusted for the child and family context.
Final thoughts: progress, not perfection
Download the graphic here.

Managing type 1 diabetes in children under five is one of the hardest jobs in diabetes care. With consistent routines, tailored insulin strategy, and early adoption of CGM and AID systems, many families can move towards over 70% time in range and over 50% in tight range — safely and sustainably. [3–5]
Success does not come from perfection. It comes from iteration, structure, and the long game.
Please share with those who may benefit.
Produced by the GNL Team with lots of help from Louise Collins, RN, and Dr Ruth Krone at the Birmingham Children’s Hospital.
Resources
Use these when you want the deeper playbook, common questions, or the next layer of system-building:
- Mastering CGM (10 top)
- Top 10: Optimise time in range with AID systems
- Bolus insulin and pre-bolusing
- Carbohydrate counting
- Meal insulin guide (infographic)
- Download: Mastering Glucose Control Under-5s (PDF)
References
- [1] Rawshani A, et al. Early-onset type 1 diabetes and long-term risk outcomes (Lancet). PubMed
- [2] Cameron FJ, et al. Hyperglycaemia and brain development/cognition in young children with T1D. PubMed
- [3] ISPAD Clinical Practice Consensus Guidelines: glycaemic targets in paediatric T1D. PubMed
- [4] Early continuous glucose monitor use in young children and observed TIR. Diabetes Care
- [5] Effect of long-term closed-loop insulin delivery in young children (TIR outcomes). Diabetes Care
- [6] German Diabetes Prospective Follow-up Registry (DPV): insulin requirement variability in under-6s. PubMed


Great advice!